Dr. Marcus Ettinger B.Sc., D.C. “Since 2007 – The Original H. pylori Treatment Protocol™”
DISCLAIMER: This post on H. pylori is for educational purposes only. This post is not a recommendation, recipe, or guide for self-treatment. Nothing in this post is designed to offer treatment recommendations or aid in a diagnosis of a particular disease or symptom. Ettinger, Inc.; Dr. Marcus Ettinger, or www.advancedhealing.com is not responsible for or to be held liable for the reader using or not using any part of this post. Lastly, please seek medical attention or call 911 if you are experiencing a medical emergency.
Important Note: To receive protocol information or coaching for H. pylori, SIBO, and biofilm or related health issues… you will need to become an in-office or distance patient – Policies and Fees. I want to help you and I can create a tailor-made protocol for your situation. Please call for a complimentary 15-minute consultation to see if we are a good fit – 714-639-4360.
Table of Contents
- Introduction
- My Predisposing Factors
- So What Was the True Cause of My Gastritis?
- Diagnostic Testing
- The True Cause Was H. pylori:
- Flys – An Unexpected Route For H. pylori Infection
- H. pylori Treatment Protocol
- H. Pylori Articles
- Important Protocol Updates:
- H. pylori In The News
Introduction
H. pylori infection can cause gastritis, ulcers, heartburn, SIBO, anemia, low stomach acid, Insulin resistance, rosacea, anxiety, depression, chronic fatigue, and more.
“Heartburn, chronic active gastritis, GERD, acid reflux, achlorhydria or H. Pylori – that is the question.” William Shakespeare. Are any of these conditions actually due to too much stomach acid (hyperchlorhydria)? Not necessarily and rarely so. I have to admit here, that I experienced an acute and severe bout of gastritis when I started my first practice. And yes, it hurt, bad! It felt like someone poured a quart of battery acid down my throat, at the same time I was having a heart attack while licking a brand-new nine-volt battery. I think you get the picture.
Well, to make a long story short, my stress wasn’t going to go away in the next five minutes. I needed to apply my “medical detectiveness” and reverse engineer what was going on based on the pathophysiology of the condition, to figure out the cause. Knowing the cause and predisposing factors would allow me to apply the precise heartburn treatment, H. pylori treatment, chronic active gastritis treatment, GERD treatment, or low stomach HCl treatment. The cause and/or predisposing factors were:
My Predisposing Factors
1. Chronic Dehydration – There are different types of mucous cells in the stomach, as well as the small and large intestines, and they are easy sources to supply the body with water when dehydrated. The thinning of the gastric mucosa or destruction of that mucous membrane layer makes the stomach vulnerable to organic acids – hydrochloric or those produced from the fermentation of ingested sugars and purification of ingested proteins. Decreased stomach acid (HCl) due to being locked in a flight-flight mode contributed to the perfect storm for the introduction and/or colonization and/or activation of the dreaded H. pylori bacterium.
Phases of Digestion Series
Part 1 of the 5 Phases of Digestion – How Our Stress Level Affects Digestion And Assimilation
Parts 2 and 3 of the 5 Phases of Digestion – The Mouth and The Stomach
Part 4 of the 5 Phases of Digestion – The Small Intestine
Part 5 of the 5 Phases of Digestion – The Large Intestine/Colon
2. Zinc Deficiency – I picked up on this during a hair mineral analysis. Zinc deficiency as a singular factor would, most likely, not cause anything overtly noticeable. When combined with a Helicobacter pylori (H. pylori) infection, the compounding effects created a more severe inflammatory reaction within the gastric lining.
3. One Bourbon, One Scotch, One Beer – Ethanol on its own can create painful erosion and inflammation of the gastric lining, but when combined with zinc (and B1) deficiency, it can compound the degree of inflammation and drastically delay healing.
4. H. pylori or Lack of HCl? – After testing, it was confirmed that H. pylori was present. Now was my lack of HCl the reason I got the H. pylori or was the H. pylori the cause of the reduced stomach acid? At this point, it didn’t matter because I couldn’t take HCl due to gastritis and further research showed that the H. pylori bacterium does indeed lower HCl levels (neutralize) in the stomach.
So, to make a long story short, not only was I up shit-creek without a paddle, but I was missing the canoe too.
So What Was the True Cause of My Gastritis?
#1, #2, #3, and #4 all played their individual parts in my condition. A little more on #4 – Achlorhydria (lack of stomach HCl) or H. pylori bacteria: This is the, what came first, chicken or the egg dilemma. Did my lack of stomach acid allow the H. pylori a safe haven to take up residence or did the H. pylori infection cause the lack of stomach acid? Both are possible and both allow the other to exist and create a painful condition called atrophic gastritis. This is exactly what I had, and, I am sure, a little erosive gastritis as well.
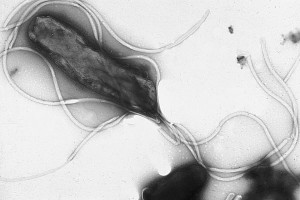
H. pylori bacteria
Diagnostic Testing
After some diagnostic testing: allopathic (traditional medicine), which included Diagnostic Solutions GI-MAP (GI-MAP | GI Microbial Assay Plus w/ H. pylori Antigen and Virulence Factors – $425) and energetic testing (Applied Kinesiology & Contact Reflex Analysis), I now knew what was going on, what caused it and what to do to get it completely under control. It was confirmed I did have Helicobacter pylori – H. pylori for short.
Urea Breath Test vs Stool Antigen Testing – The Prefered Method of Testing
The H. pylori Urea Breath Test (30C UBT) is a sensitive and specific method for the non-invasive detection of H pylori infection, but gastric bacterial overgrowth may lead to a false positive diagnosis. Patients with low to no hydrochloric stomach acid can present with many urease-positive bacteria other than H. pylori. The strong urease activity may be responsible for false positive results of an H. pylori Urea Breath Test in patients with suspected H. pylori infection.
References:
Urease-positive bacteria other than Helicobacter pylori in human gastric juice and mucosa.
Gastric bacterial overgrowth is a cause of false positive diagnosis of Helicobacter pylori infection using 13C urea breath test
The True Cause Was H. pylori
One of our oldest companions is a microbe called Helicobacter pylori, or just H. pylori. It has been colonizing our stomachs and co-evolving with us, for the past 50,000 – 100,000 years. Helicobacter pylori (H. pylori) is a spiral-shaped gram-negative bacterium that was identified in 1979[1].
H. pylori, in those infected, can thrive in their gastric epithelium and in the very thin layer of overlying mucus that protects the stomach wall from the stomach’s hydrochloric acid, a special niche that is hostile to nearly all other microbes. One mechanism by which the bacterium does this is by producing urease in abundance. It is reported that urease functions in H. pylori infection to neutralize gastric acid by producing ammonia (NH3). Enhanced production of NH3 also may facilitate the formation of NH3-derived compounds, such as monochloramine, which shows cytotoxic effects on host cells. Enhancement of bacterial motility and inhibition of phagocytic clearance of bacteria were also reported as functions of urease.[6]
About half of the world’s population house H. pylori, in their stomach, and are unphased by it. But in about 10-15 percent of those infected, the microbes cause peptic ulcers and chronic active gastritis, and in an unluckier bunch, about 2%, the H. pylori is a causative agent for gastric (stomach) cancer and mucosa-associated lymphoid tissue lymphoma[2]. It has also been shown to be associated with extra-gastric diseases, such as
It has also been shown to be associated with extra-gastric diseases, such as unexplained refractory iron deficiency anemia and idiopathic thrombocytopenic purpura[3-5].
“Everybody with Helicobacter does have inflammation or some irritation in the lining of the stomach and because it lasts your whole life it gradually builds up. This means Helicobacter needs to be treated in people, even if they do not feel unwell.” Professor Barry Marshall. Both Emeritus Professor Robin Warren and Professor Barry Marshall received the Nobel Prize in 2005 for discovering the bacteria Helicobacter pylori (H. pylori).
- Pajares JM, Gisbert JP. Helicobacter pylori: its discovery and relevance for medicine. Rev Esp Enferm Dig 2006; 98: 770-785
- Sari YS, Sander E, Erkan E, Tunali V. Endoscopic diagnoses and CLO test results in 9239 cases, prevalence of Helicobacter pylori in Istanbul, Turkey. J Gastroenterol Hepatol 2007; 22:1706-1711
- Bohr UR, Annibale B, Franceschi F, Roccarina D, Gasbarrini A. Extragastric manifestations of Helicobacter pylori infection — other Helicobacters. Helicobacter 2007; 12 Suppl 1: 45-53
- Franceschi F, Roccarina D, Gasbarrini A. Extragastric manifestations of Helicobacter pylori infection. Minerva Med 2006;97: 39-45
- Franceschi F, Gasbarrini A. Helicobacter pylori, and extragastric diseases. Best Pract Res Clin Gastroenterol 2007; 21: 325-334
- Hideo Kuwahara, et. al., Helicobacter pylori Urease Suppresses Bactericidal Activity of Peroxynitrite via Carbon Dioxide Production. Infect Immun. 2000 Aug; 68(8): 4378–4383.
Flys – An Unexpected Route For H. pylori Infection
By Kristin Hugo: The flies in your home, at your picnic, and at the local food court may be even grosser than you thought. A new study finds that they are crawling with bacteria and even host diseases that could be harmful to humans.
Researchers at Penn State collected 116 blowflies and houseflies from different habitats in Brazil, Singapore, and the United States. They sampled urban sites such as a food market and a hospital emergency entrance, rural sites including farms, and natural sites such as the Amazon Rainforest. In addition to the wild-caught flies, they also sampled control flies from a colony of blowflies that had been captive-bred for 20 generations. They found that the bodies of the animals, especially the wild-caught ones, were covered in bacteria—including bacteria that can be harmful to humans.
Most bacteria found on the flies wouldn’t be able to infect a human host, but Helicobacter pylori can live in your gut for years and then form ulcers and could, according to some research, increase the risk of stomach cancer. The researchers found virulent strains of the bacteria on several blowflies. However, they also noted that the chance that you could be adversely affected by this microbe is highly dependent on how susceptible you are to infection. Half of the world’s population already has this bacteria in their gut, but it’s not clear how many people got the infection from flies.
After collecting the wild-caught flies, the researchers sequenced the genomes of the life found on their respective bodies. They found that the wings and legs of the animals had the most microbial diversity or different types of microbes living on them. Surprisingly, the flies collected from urban environments were covered with even more pathogens than those collected from stables. The research was published in the journal Scientific Reports.
It shouldn’t be too surprising that flies might carry pathogens. Flies aren’t known for their attraction to cleanliness and prefer to lay their eggs on rotting carcasses and in feces. However, they do keep themselves clean enough. If you’ve ever seen a fly rubbing its legs together and scrubbing its face, that fly was actually cleaning itself, just as a cat or mouse would.
H. pylori Treatment Protocol
The Original H. pylori Pre-treatment – First, I took antacids (over-the-counter – Zantac OTC, an H2 blocker) to increase the susceptibility of the H. pylori to treatment (eradication), lessen the need for H. pylori to defend itself so vigorously, and to allow my gastric mucosa a chance to heal. At least that was my thinking at the time. Note: H. pylori forms protective bacterial colonies called biofilm, which is made up of a protective, extracellular polysaccharide shield. This protective shield is a defensive barrier against stomach hydrochloric acid and other substances, like antibiotics. Being a complex matrix of proteins and carbohydrates, which are probably interdependent, the H. pylori biofilm could possibly offer a protective haven for the survival of this gastric bacterial pathogen in the extra-gastric environments (Proteomannans in Biofilm of Helicobacter pylori ATCC 43504). As well as Candida albicans and other bacteria.
The Current H. pylori pre-treatment consists of a personalized, 30-day BIOFILM PROTOCOL and Gut Restoration Protocol. Since H. pylori bacteria can produce a biofilm and is, day by day, becoming more immune to conventional antibiotics, I have found it quite helpful to weaken its outer defenses before the Marines (natural antimicrobial agents and antibiotics) are sent in.
The Original H. pylori Treatment – Second, my personal H. pylori bomb consisted of Monolaurin (lauric acid) or Lauricidin – also see coconut oil, which is 50% lauric acid by weight) and H-PLR (K-32) (Supports bacterial elimination) from Apex Energetics. I also juiced 1/4 cabbage every day (cabbage contains S-Methylmethionine known as Vitamin U; a great healer of ulcers and gastritis). After 4 weeks of my protocol, I was feeling like a new man! I re-checked myself, after 8 weeks (stool test), and was free of the foreign invaders, a breath test confirmed the same.
The Current H. pylori Treatment consists of either the Prevpac, Omeclamox®-Pak, or Pylera pharmaceutical regime minus the PPI (Please read the August 2014 update below, for clarity) and a personalized combination of natural antimicrobial agents. Below are the products I’m currently pulling from to create an individualized H. pylori protocol. Having the correct biofilm and H. pylori protocol IS just as important as having the correct therapeutic dosage of the products being used. The degree that the balance of the three is off is to the degree that the entire protocol may fail. This is why it is always best to have a qualified coach and to never self-treat.
- Pylopass (no longer available) H. Pylori Fight by Super Smart is what is available now – LEARN MORE ABOUT PYLOPASS – “Pylopass Eliminates H. pylori with Confidence”
- Black Seed Oil (Nigella Sativa)
- H-PLR and/or Bio-HPF and/or Berbemycin.
- S. boulardii
- Bladderwrack and/or Cranberry Extract w/D-Mannose
- Ulcetrol/Gastro Comfort and/or Gastrazyme
- A More Streamlined Version Of The Personalized Biofilm Protocol
- A Personalized Version Of My Health Restoration Shake
- Lifestyle Modification
Below are the products I don’t use or recommend as part of a natural H. pylori protocol. It’s not that these are bad products, in and of themselves. I’ve just found them to be weak or not effective.
- Mastic Gum
- Matula tea
- Manuka Honey
Note: As of September 2009, I’m also adding Klaire Labs – InterFase Plus (use under a doctor’s supervision or recommendation) or InterFase, to my H. pylori treatment protocol. InterFase Plus or InterFase is now an important and mandatory part of the protocol. InterFase Plus or InterFase aids in the eradication of biofilm, especially H. pylori biofilm colonies. This is a major advancement in my protocol. Understanding what BIOFILM is is extremely important for a variety of reasons. Please follow any biofilm link to read more about it. Also, read about my biofilm protocol – please do not self-treat. Additional products that can be taken during the treatment phase: VSL#3 or Probiotic-10 (multi-strain probiotic and prebiotic formula), NAC by Now Foods, S. boulardii, and Psyllium Husk Fiber (not for SIBO patients). Also, my Biofilm Protocol is integrated into the H. pylori elimination Protocol.
Certain dietary restrictions and additions will need to be taken. These are determined on a case-by-case basis. The two that are required for everyone are: avoid all cow’s milk and gluten-containing products.
Prevention and Healing – Lastly, I needed to keep the H. pylori bacteria from coming back and keep the healing process moving forward. I took pancreatic enzymes w/HCl* and plant-based with each meal, zinc** and L-carnosine** Ulcetrol from Now Foods has both of these. Mastic gum***, TheraAloe****(No longer available), chlorella and/or spirulina, a daily broad-spectrum probiotic (VSL#3 or Probiotic-10 from Now Foods), NAC, psyllium husk fiber and tons of distilled water, for 6 weeks. I was now better than before my first symptom.
All-in-all, it was a learning experience and one that has made me a better doctor and a more diligent medical detective.
FYI: Gastritis is not a single condition, but several different conditions that all share inflammation of the stomach lining as a common symptom. Gastritis, most often, is caused by prolonged use of non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or aspirin, chronic dehydration, drinking too much alcohol, or infection such as Helicobacter pylori bacteria (H. pylori). It may also occur after major surgery, severe infections, trauma injury burns, or severe infections. Some diseases, such as pernicious (B12 deficiency) anemia, autoimmune diseases, and chronic bile reflux, can cause gastritis as well.
*Microscopy studies of the motility of H. pylori in gastric mucin at acidic and neutral pH in the absence of urea show that the bacteria swim freely at high (alkaline – achlorhydria) pH, and are strongly constrained at low (acidic) pH. Also, H. Pylori, through enzyme reactions promotes increased ammonia production, which raises the pH of its environment – allowing it to move more freely.
**A combination of zinc and L-carnosine has been shown to prevent gross visible damage to gastric mucosa caused by ethanol ingestion. This combination also acts as a potent antioxidant, specifically benefiting the gastric mucosa. Polaprezinc, a mucosal protective agent, in combination with lansoprazole, amoxicillin and clarithromycin increases the cure rate of Helicobacter pylori infection
***There is conflicting data on whether mastic gum kills H. pylori effectively in vivo (live human trials). Killing it in a test tube or mice is one thing, but I am interested in living human beings. There is evidence that it aids in the healing of the gastric mucosa, possessing anti-inflammatory properties. I used it for healing rather than as an agent to kill the H. pylori bacteria. Note: there are studies that have shown that mastic gum kills H. pylori. The problem is that it is less than 30% of the trial groups. So it works in about 1 out of every 3 that try it as a primary treatment (at dosages of 500 mg 3x/day).
****TherAloe is a high molecular weight polysaccharide containing aloe vera juice product. Its healing capabilities, as far as I am concerned, are quite profound on the gastric mucosa.
H. Pylori Articles
- Helicobacter pylori Facts and More Facts…
- Blog post – H. pylori-free, in just 34 days, without antibiotics.
- H. pylori Treatment Testimonial – 03/2018
- Lactobacillus gasseri For H. pylori Eradication
- Natural H. pylori Treatment Worked Even After Antibiotics Failed
- Herbs, Probiotics, and H. pylori
- Biofilm Basics
- Dr. Ettinger’s Biofilm Protocol for Lyme and Gut Pathogens
- Quorum Sensing and Biofilm
- Can H. pylori actually be good for us? An Endangered Species in the Stomach, by Martin J. Blaser
- Probiotics May Represent a Novel Approach to The Management of H. pylori Infection.
- Helicobacter Pylori and Alzheimer’s
- Ulcer-Causing Helicobacter Pylori Survives In Our Acidic Gut By Turning It Neutral
- Antibiotics Have Turned Our Bodies From Gardens Into Battlefields – an interview with microbiologist, Dr. Martin Blasser
- Helicobacter pylori and cardiovascular complications: a mechanism-based review on the role of Helicobacter pylori in cardiovascular diseases
- The bacterial virulence factor CagA induces microbial dysbiosis that contributes to excessive epithelial cell proliferation in the Drosophila gut.
Important Protocol Updates
PLEASE READ 19 August 2014 Updated, Update – (Original: 08 Aug 2013): Why H. pylori Infections Are So Hard To Treat – I have been helping patients with H. pylori, a biofilm-producing bacteria, for almost 7 years now. In the beginning, eradicating this bug was very easy, in my opinion. As time progressed I noticed that the same protocol I had been using was becoming less and less effective – on first-timers, not re-treatments. There are now H. pylori strains that are now multiple drug-resistant. Medically there is no real explanation for this. Energetically there is a very good explanation, for me anyway, based on the research done by Rupert Sheldrake, Ph.D. on Morphic Fields and Morphic Resonance. Please read about his theory for further clarification.
Because of this new shift in loss of effectiveness, in some patients, I have had to use more than one round of products or add more products to the protocol. The end result has always been eradication but it’s now taking more to achieve this result. Also, there are many people contacting me and letting me know that they have undergone triple and quadruple therapies to no avail. This proves in my mind that biofilm and the bacteria that create them are learning to defend themselves more effectively. They are adapting and mutating, genetically, to survive. Good for them and bad for us.
My theory is that with the introduction of hundreds of blogs, chat rooms, and websites devoted to H. pylori and biofilm, more and more people are self-treating. This self-treating is not killing the H. pylori or eliminating the biofilm but on the contrary, makes them both stronger by building up the biofilm defense. Every time a bacteria that produces a biofilm is unsuccessfully treated it becomes more resistant to the next protocol. When this is combined with the theory of Morphic Fields, it’s no wonder that H. pylori and biofilm eradication is becoming harder and harder to achieve. The point of all of this is that there are still effective treatment options available, it may just take a little more time and/or more products, allopathic (Prevpac or Pylera) and/or natural to get to the desired end result – H. pylori and biofilm eradication.
Lastly, I am not against self-treating per se. The issue is that the information, on the web, on biofilm and H. pylori, is not comprehensive or clear enough for the layperson to be their own doctor or to successfully self-treat. I have always advocated and promoted that if you want to get better with or at something, you need a coach who is an expert in that field or subject. There are times and places where self-help is good, but biofilm and H. pylori treatment are not one of them. This is just my opinion.
PLEASE READ 24 July 2018 Update – Why Not To Use Proton Pump Inhibitors (PPIs) – A study published in the journal Gut identified an association between long-term use of PPIs and a 2.4 times higher risk of developing stomach cancer. A link between PPIs and a higher stomach cancer risk has previously been identified by academics – but never in a study that first eliminates a type of bacteria suspected of fuelling the illness’s development. Research by the University of Hong Kong and University College London found that even after H. pylori was removed, the risk of developing the disease still rose in line with the dose and duration of PPI treatment.
Gastric cancer is the fifth most common cancer and the third most common cause of cancer-related death in the world. It is now well-established that Helicobacter pylori infection predisposes individuals toward gastric adenocarcinoma later in life. It has since been classified as a class I carcinogen by the World Health Organization. Research suggests that the oncogenic effects of Helicobacter pylori can occur through a variety of mechanisms, including the indirect inflammatory effects of Helicobacter pylori on the gastric mucosa and the direct epigenetic effects of Helicobacter pylori on individual cells.
H. pylori In The News
July 24, 2018 Update – H. pylori has several virulence factors that interact with specific targets in the cell and directly affect the severity of gastric disease. Vacuolating cytotoxin A (VacA) was previously the only main H. pylori factor known to act on mitochondria, causing cellular membrane and organelle dysfunction, ultimately leading to cell death.
Scientists from the Institut Pasteur and the CNRS have discovered that H. pylori uses at least two additional strategies to target mitochondria. These strategies do not lead to cell death but maintain an environment that is conducive to bacterial proliferation.
Their results show that H. pylori affects both mitochondrial transport systems (used to transfer proteins into mitochondria) and the machinery for the replication and maintenance of the mitochondrial genome. The scientists also discovered that contrary to what was previously believed, VacA is not the only H. pylori component capable of affecting mitochondria. This suggests that the bacteria may produce other mitochondria-interacting factors that have not been yet identified.
Co-author Miria Ricchetti of the Institut Pasteur says, “The damage to mitochondria caused by H. pylori bacteria is temporary and disappears once the infection has been eliminated. Despite remarkably high levels of stress, mitochondria, like cells, can remain functional and withstand infection for longer than previously thought. It is important for us to bear this in mind when looking for strategies to inhibit the bacterium’s pathogenic potential.”
For the first time, scientists have found that the binding of the bacteria to the stomach mucosal layer is acid-sensitive, allowing it to attach and detach when needed.
The bacteria bind to the mildly acidic (pH 6) mucous layer of the stomach and when the mucous is shed into the highly acidic (pH 2) stomach, the bacteria quickly unbind and move to a fresh mucous layer site.
Breakable binding: Previous studies have shown that the bacteria tightly attach to the epithelial cells and mucous of the stomach with the help of an adhesin called BabA. But now the researchers found that though tightly bound to the mucous, the binding affinity reduces once the bacteria sense more acidic pH (2-4 pH). The mucous lining of the stomach is constantly shed into the stomach, which is highly acidic compared with the mucous layer.
The scientists found a 2- and 20-fold less binding at pH 4 and 2, respectively, compared to pH 6. Within 30 seconds, 85% of the bacteria detached from the mucous layer when placed in a strong acid. They also saw that 95% of them recovered binding activity when shifted to a less acidic site.
“Such a pH-dependent, reciprocal attachment-detachment system should be a great advantage for long-term colonization in the stomach. Indeed, its importance is supported by the extensive microevolution of BabA,” Dr. Asish K. Mukhopadhyay from the National Institute of Cholera and Enteric Diseases (NICED), Kolkata says in an e-mail to The Hindu.
In order to know the exact pH at which bacteria lose binding, they tested 21 Swedish bacteria isolates. They found that the bacteria detached at pH ranging from 2.3 to 4.9 showing that they can adapt to individual acid secretion patterns. Dr. Asish Kumar Mukhopadhyay in an Article for The Hindu
Research shows how H. pylori bacteria can cause neutrophils, a type of white blood cell, to morph
“The concept of neutrophil plasticity is new and, to our knowledge, these data are the first evidence that neutrophils can undergo subtype differentiation in vitro in response to bacterial pathogen infection. We hypothesize that these changes favor H. pylori persistence and disease.” March 1, 2017, in the Journal of Immunology
Antibiotic resistance among Helicobacter pylori clinical isolates in Lima, Peru
Results: Seventy-six isolates were recovered from gastric biopsies. Clinical isolates showed evidence of antibiotic resistance to 1 (27.6%, n=21/76), 2 (28.9%, n=22/76), or ≥3 antibiotics (40.8%). Of 76 isolates, eight (10.5%) were resistant to amoxicillin and clarithromycin, which are part of the standard triple therapy for H. pylori infection. No trends were seen in the presence of cagA, vacA m1, or vacA m2 and antibiotic resistance.
Conclusion: The rate of antibiotic resistance among H. pylori isolates in Lima, Peru, is higher than expected and presents cause for concern. To develop more targeted eradication therapies for H. pylori in Peru, more research is needed to better characterize antibiotic resistance among a larger number of clinical isolates prospectively. Infection and Drug Resistance, March 10, 2017
Helicobacter pylori Adapts to Chronic Infection and Gastric Disease via pH-Responsive Protein Adhesion Molecule
For H. pylori to thrive in the acidic environment of the stomach, the gastric pathogen uses a specific protein to attach to the protective pH-neutral mucous lining. New research shows how a specific adhesin protein has a pH-responsive mechanism allowing H. pylori to rapidly detach from old cells before they reach the brunt of the gastric acid. The release mechanism lets the bacteria return to the pH-neutral mucous lining and recycle the chronic infection. The Umeå University-led research findings are published today in Cell Host & Microbe Cell Host & Microbe, March 08, 2017
Helicobacter pylori infection significantly increases insulin resistance in the asymptomatic Japanese population.
Helicobacter pylori infection has been shown to contribute to atherosclerosis and cardiovascular diseases. Insulin resistance is the pathophysiologic background of the clinical features of atherosclerosis and cardiovascular diseases. Helicobacter, October 14, 2009
The Association Between Helicobacter pylori Infection and Insulin Resistance: A Systematic Review. Although data seem to indicate a potential association between H. pylori infection and IR, further studies are needed to strengthen this association and to clarify whether there is a causative link between them. If a causal link is confirmed in the future, this may have a major impact on the pathophysiology and management of IR syndrome, including type 2 diabetes mellitus and nonalcoholic fatty liver disease. Helicobacter. April 16, 2011
September 13, 2009, Update – I am now taking, Source Naturals – Broccoli Sprouts Extract, which provides 2,000mcg’s sulforaphane daily. This is equivalent to eating more than a pound of fresh broccoli. Dietary Sulforaphane-Rich Broccoli Sprouts Reduce Colonization and Attenuate Gastritis in Helicobacter pylori–Infected Mice and Humans
October 03, 2009, Update – H. pylori most likely will live in biofilm colonies which make them even harder to kill or be identified by our host defenses. Read more about biofilms here and my protocol to remove them. BIOFILM
November 03, 2009, Update – In my never-ending quest for knowledge, I just came across this interesting piece of data. The H. pylori bacteria is thought to have been with us for around 58,000 years and migrated with modern man out of East Africa. Here is the link to this article. – An African origin for the intimate association between humans and Helicobacter pylori
November 18, 2009, Update – Here are two PubMed articles validating the effectiveness of Monolaurin for the prevention and/or eradication of H. pylori.
Int J Antimicrob Agents. 2002 Oct;20(4):258-62
Bactericidal effects of fatty acids and monoglycerides (Monolaurin) on Helicobacter pylori
Bergsson G, Steingrímsson O, Thormar H. Institute of Biology, University of Iceland, Grensasvegur 12, 108, Reykjavik, Iceland. bergsson@here.is
The susceptibility of Salmonella spp., Escherichia coli, and Helicobacter pylori to fatty acids and monoglycerides was studied. None of the lipids showed significant antibacterial activity against Salmonella spp. and E. coli but eight of 12 lipids tested showed high activity against H. pylori; monocaprin and monolaurin being the most active. The high activity of monoglycerides against H. pylori suggests that they may be useful as active ingredients in pharmaceutical formulations.
Mol Cell Biochem. 2005 Apr;272(1-2):29-34
Minimum inhibitory concentrations of herbal essential oils and monolaurin for gram-positive and gram-negative bacteria
Preuss HG, Echard B, Enig M, Brook I, Elliott TB. Department of Physiology and Biophysics, Georgetown University Medical Center, Washington, DC 20057, USA. preusshg@georgetown.edu
New, safe antimicrobial agents are needed to prevent and overcome severe bacterial, viral, and fungal infections. Based on our previous experience and that of others, we postulated that herbal essential oils, such as those of origanum, and monolaurin offer such possibilities. We examined in vitro the cidal (def. killing, as in bactericidal) and/or static effects of oil of origanum, several other essential oils, and monolaurin on Staphylococcus aureus, Bacillus anthracis Sterne, Escherichia coli, Klebsiella pneumoniae, Helicobacter pylori, and Mycobacterium terrae. Origanum proved cidal to all tested organisms with the exception of B. anthracis Sterne in which it was static. Monolaurin was cidal to S. aureus and M. terrae but not to E. coli and K. pneumoniae. Unlike the other two gram-negative organisms, H. pylori was extremely sensitive to monolaurin. Similar to origanum, monolaurin was static to B. anthracis Sterne. Because of their longstanding safety record, origanum and/or monolaurin, alone or combined with antibiotics, might prove useful in the prevention and treatment of severe bacterial infections, especially those that are difficult to treat and/or are antibiotic resistant (also see biofilm, as a source of antibiotic resistance).
Note: Monolaurin has been shown to inactive many forms of bacteria and viruses that are protected by an outer lipid membrane, known as an envelope (H. pylori cell envelope). The mechanism is due to monolaurin’s ability to aid in the disintegration of this lipid membrane.
May 02, 2010 Update – A recent review, just published, of available literature on the use of probiotics in the treatment or prevention of H. pylori infection, validated that, “Both in vitro and in vivo studies provide evidence that probiotics may represent a novel approach to the management of H. pylori infection.”
Helicobacter. 2010 Apr;15(2):79-87.
Role of probiotics in pediatric patients with Helicobacter pylori infection: a comprehensive review of the literature.
Lionetti E, Indrio F, Pavone L, Borrelli G, Cavallo L, Francavilla R. Department of Paediatrics, University of Catania, Catania, Italy. elenalionetti@inwind.it
March 28, 2011 Update – Helicobacter pylori infection has been associated with diverse extra-digestive morbidity, including insulin resistance (IR) syndrome (1), atherosclerosis, and cardiovascular diseases (2). Insulin resistance is the pathophysiologic background of the clinical features of atherosclerosis and cardiovascular diseases. Morbidity – The rate of incidence of a disease. (Medicine / Pathology) Also called morbidity rate the relative incidence of a particular disease in a specific locality.


Does the Simple Carbohydrate Diet (SCD) work for H. pylori?
The SCD will not by itself eradicate H. pylori.
Saw your notation on sulforaphane. Several years ago I began taking MSM, another sulfur-containing supplement, daily. I’m a backpacker and benefit greatly from the restoration of sulfur into tendons, ligaments. An interesting side effect emerged at 2.5 g/day: enhanced overall bacterial control. Chronic bad breath, SIBO symptoms, and lifelong rosacea-based adult acne all attenuated. Complete eradication at 1 g/ tid (165 lbs) which I still take to this day with no negative effects on digestive bacteria (which is fascinating). Sulfur is a key molecule in most non-exotic anti-bacterials and some anti-fungals. I surmise that the body, given a super-nutritional amount of S can wield it as a selective weapon against unwanted invaders.
Dave,
Great story. As an FYI, I take 1 heaping tablespoon per day. That’s between 14-16 grams depending on how heaping I go. I don’t plan on stopping. I also know a supplement formulator who takes 2-3 tbsp/day and has so for years. I’m sure some don’t don’t do well with it, but most do.
Dr. Ettinger
Hi Dr. Marcus
What daily dose and brand of Black Seed Oil supplement do you use?
Luis,
Im sorry but I do not give dosing recommendations to non-patients. I have posted that fact at the top of many of my blog posts.
Respectfully,
Dr. Ettinger
Hello Dr Marcus
What supplement do you use from Black seed oil and Cranberry?
Do you have a favourite?
Thanks!
Jorge,
It sounds like you are self-treating. That will never be a recommendation of mine, especially for one of the hardest things to treat, H. pylori.
I have no favorite brand of either of those supplements.
Dr. Ettinger
I had acid reflux for over an year. Taking prilosac for just 14 days together with manuka honey started causing me burps and foul smelling gas. I had not taken prilosac for more than 10 years. After about a month the foul smelling gas stopped but the burps are not going away.
Can H Pylori become worse with prilosac? Why would taking prilosac cause burps to start
As a general rule, Prilosec should not make H. pylori infection worse.
Prilosec reduces stomach acid. Food will ferment and putrify in the stomach as it is staying in there longer. This may be one reason for the burping. SIBO is another.
Respectfully,
Dr. Ettinger
Hi Dr Ettinger, I’ve been reading much of your posts and webpage regarding Hpylori, SIBO, gastritis etc and did a GI map test 2 years ago diagnosing Hpylori, SIBO and Candida, treated HP with triple action ABS/PPIs & some Candida protocol too but i suspect HP is back or gastritis ..i realize new testing is required. I am wondering if you know of any Drs or FMDs in Canada that you could recommend for this as you cannot order testing here nor can I afford the American $$ conversion. Thanks kindly.
Karen,
I’m sorry to hear that you’re still having problems after a full pharmaceutical protocol. I find that it takes a combination of a comprehensive natural plus pharma protocol to beat H. pylori. That said, I have not seen your GIMAP and there could be more underlying issues than just the H. pylori bacteria.
Lastly, I have no resources in Canada.
I wish you the best in finding the answers you are looking for.
Respectfully,
Dr. Ettinger
Hi Dr.Marcus!
Betaine HCL can be taken if you are positive for H.Pylori (I have not had ulcer problems)???
Taking it would help to eradicate H.Pylori???
I have GERD and when it goes up I don’t feel acid, so I think my Stomach Acid is low and that causes indigestion.
Thanks!
Jorge,
Four billion people have H. pylori right now. The vast majority of them have no symptoms and require no treatment. Those people should be okay taking Betaine HCl. If the H. pylori are creating ulcers or erosive gastritis, no HCl should be taken and the H. pylori should be treated.
Taking HCl does not help with erradication.
Dr. Ettinger
Hello Dr Marcus!
Which 13C urea breath test is better???
The one where you only drink urea or the one where you drink a citric acid solution 10 minutes before taking the baseline sample (in addition to taking urea after)???
Jorge,
The 13CO2 test is good enough. Personally, I prefer and only use stool testing by Diagnostic Solutions. This way I can qualify the level of H. pylori present, if any, and if any virulence factors are elevated. Just because it’s in you does not mean it needs to be treated.
Respectfully,
Dr. Ettinger
I did the diagnostic solutions, what would qualify for treatment? My Stool test showed H.Pylori was 1.63, negative on all virulence factors. High in gluten & zonulin. Problem is hives when I eat high histamine…from low stomach acid (took PPI’s for a few years), but Betaine makes hives worse, how do I fix food sensitivity from low stomach acid? ACV & bitters don’t work either. Thank you.
Tammie,
What would qualify for treatment? Wanting to be helped/treated. I help people all over the world. Trial and error (self-treat) is most often futile unless you have a background in biochemistry and/or physiology. How you improve on something? Hire a coach. All of the best in the world got there because of mentors and coaches. Never settle.
Respectfully,
Dr. Ettinger
Hi, Marcus!
I’m wondering how long you wait to re-test patients after treatment to avoid a false negative test.
Thanks in advance.
Tomas
The longer you wait the more accurate the test. 45 days would be good.
Hello dear Dr. Marcus Ettinger,
I like your site and thanks all for the information. But for H.pylori eradication, there is something missing. I don’t believe that this bacteria is the cause of all gastritis and ulcers. This misconception alone created chaos in the medical world. For example, tooth infection, tonsils, ear infections, appendicitis can cause gastritis and even ulcers of the stomach. My point is that focus too much on the stomach maybe can lead to danger. Also it could mean someone could have H.pylori but his ulcer is caused by a foci of infection in the neck, mouth, ears, appendice, gallbladder. And thinking that H.pylori is the cause only because it was found will lead to ignoring other causes of infections that can cause ulcers and gastritis.
The second point, the treatment I think is very simple. Fasting and taking a fiber like psyllium husk from 1 week to 20 days will completely cure H.pylori. The French Immunologist Bruno Donatini used only one mushroom by immunomodulation cured most gastritis and cleared H.pylori and it was Lion’s mane mushroom.
Yahia,
You are correct. There are many causes of gastritis and ulcer. Most of the people that contact me for help with H. pylori don’t receive an H. pylori protocol. After working them up we find that their GI issues are caused by something else and H. pylori just happens to be present, but not active.
As far as your second point, I’m highly suspicious about psyllium and lion’s mane being so powerful against H. pylori. I have been treating H. pylori for over 15 years and know it like my own right hand. As an experiment, I will treat my next, new, H. pylori patient with both psyllium and lion’s mane and pay for their follow-up test to see what happens. I’ll bet it comes back positive and will eat crow if it comes back negative. I’ll post the results in a blog post when they come in.
Respectfully,
Dr. Ettinger
Hello dear Dr. Ettinger,
Thank you for your time and your answer. I did not elaborate about psyllium and H.pylori. For Lion mane mushroom, Dr. Bruno Donatini in France who is an MD and immunologist did a clinical trial comparing Lion mane mushroom to triple therapy for H.pylori. Lion mane group eradicated H.pylori much better than triple therapy.
As for psyllium husk and fasting, There is a Russian thesis about eradicating H.pylori with IL2 injection. Psyllium husk and fasting can increase IL2 and immunomodulate the immune system. The water fast must be from 1 to 2 weeks with only psyllium husk as a fiber and Hericidium ( lione mane) mushroom.
I read a lot about fasting. It is the only rejuvenating tool. It is not dangerous as some doctors believe. There is only few diseases where fasting can be harmful like active tuberculosis. Psyllium husk will increase IL2 and reduces IL8. Also it has a soothing effect on the inflamed mucosa.
The immune system is a Beast. I think it can get rid of any microbe. Remember the Greek philosopher axiom: The whole is larger than the sum of the its parts. The immune system is far more superior to any microbe. It only needs optimal environment to work.
Also another mystery of fasting is the diet after fasting. You can use the moons of the nail as an indicative of the vitality. You have to introduce food slowly after the fast. By this you will see the moon growing in the nails. If you introduce large food and diet, not only the benefit of the fast will fade but the fasting will be unhealthy and the moons of the nails won’t grow.
H.pylori also works with herpes viruses ( Epstein barr, cytomegaloviruses, herpes simplex 1 and 2). Dr. Bruno Donatini uses medicinal mushrooms to lower the viral loads to get rid of immunosuppression by these mushrooms.
Fasting also kills all viruses by autophagy.
Hippocrates said that bodies that are not properly cleansed, the more you nourish them, the more you injure them. Diseases which arise from repletion are cured by depletion” Aphorism. It means fasting is a must to clean the body and not overnutrition as it is promoted by many health gurus. Nutrition is great but overnutrition will cause malnutrition.
I hope we learn from each other a lot. I am coming with a method of curing most infections.
Best regards,
Yahia
Yahia,
Thank you for sharing your thoughts and personal experience.
Respectfully,
Dr. Ettinger
Hi Doctor. Did you try the husk and lions mane treatment and what were the effects if so?
Dan, I have not tried those for H. pylori. Dr. E
First of, thank you very much for your time and effort you’ve put in these posts.
Dr, I’ve been suffering from gastrointestinal issues from 5 years.
I was suffering from heartburn, chronic mild gastritis (confirmed by endoscopy) with H.Pylori biopsy coming back negative and bronchitis like symptoms (mucus)
Other general and lower gastrointestinal symptoms I was suffering where:
bloating, constipation, food intolerances, brain fog, fatigue, eczema, anxiety, depression.
Went to the US to have a GI MAP and OATS Test, which indicated:
H.Pylori, Candida and obviously Dysbiosis.
I took the following treatment that my Naturopath put me in, including:
Zinc/carnosine
PYLORISTAT (Nutridyn) (two months straight)
plus some other stuff for the candida ( which is UNRESOLVED)
All symptoms subsided but I still have some bad breaht, and some mucus in the upper respiratory part which I think is biofilm.
I will start a candida protocol on my own but wanted to ask you some things.
1. How possible is to still have pylori in my case.
2. Ive read you recommend 2/2x a day 600 mg Monolaurin but what about Nattokinase and NAC dosing, any recommendations?
3. Do you still accept online international clients? This is my goal but I dont have a lot of money to spend and a consultation with you will impossibilitate me to get the medicine so Im trying to inform myself
thank you doc
Blessings from Mexico
Salomon,
I’m still accepting new patients.
Thank you.
As far as protocol recommendations go, I’m not going to give you or anyone else blind recommendations. There are tons of blogs and chat rooms dedicated to that. If you would like to build a more informed protocol, I would need all your past tests, new patients questionnaires, and we would then have a consultation. This may not be what you wanted to hear, but my 32-year reputation is at stake.
I’m here for you if you need me as one of your doctor/coaches.
Respectfully,
Dr. Ettinger
Hi,
Is it possible that I tested negative for H.pylori from stool and sample from my stomach due to taking mastic gum? I have pain and gas in the stomach with nausea and diarrhea and burping. I am desperate.
Thank you.
Kristina,
If they did both a stomach biopsy and a stool test for H. pylori and both came back negative, then I would bet you DON’T have H. pylori. There are many causes of stomach and intestinal pain. I have helped people all over the world find the “WHY” that is causing the problem and then helping them handle the problem. If interested in my help, we can have a 15-minute Zoom call to see if we are a good fit. You can email me at sibodoctor @ gmail . com
Respectfully,
Dr. Ettinger
I started suffering from this h.pylori bacteria for 4 years now . Heartburn, bloated, stomach ache will wake you up in the morning. Its so awful. I finally decided to do the triple therapy. I’m now at 6th day of doing it. I almost lost hope but thankfully I read articles like this were people successfully overcome this evil bacteria. Is it ok to also take oil of oregano while doing the therapy? I’m also a bit confuse when to take the probiotics and if we will do some juicing, is it before or after meals.? Thank you for this informative site. I hope to get well soon.
Mario,
You are welcome for any information that you may be helpful.
I can’t make recommendations to non-patients. That said, oregano oil is very safe and well-tolerated.
Respectfully,
Dr. Ettinger
Very good and informative article about H. Pylori. Thank you!
Rodolfo, Your welcome, and I hope it was helpful to you.
Hi sir I really need your help I had 2 lines antibiotics and doesn’t work and then I took matula tea after few months I took mastic gum with manuka honey the strongest one after and many different herbs but unfortunately I’m still positive I had endoscopy there wasn’t any inflammation or any things I got only reflux no any syptoms . Please I really need your help I just want back to my normal life .I really hate my life now . please help
RV,
Here is a link to my distance client application. https://www.advancedhealing.com/wp-content/uploads/Distance-Client-Program-revised-01-January-19-1.pdf
Respectfully,
Dr. Ettinger
Dr. E –
I’m so impressed with your website and knowledge. I foolishly tried to self-treat and one of the mistakes that I’d made was taking biofilm busters such as Lactoferrin, NAC, Interfase, Nattokinasse, etc for several months. Per your information – I’m concerned that they’ve built a resistance. I’m not about to start triple therapy. I’ve finally decided to throw in the towel because as much as my symptoms have drastically improved, I still have the h-pylori and I primarily use my tongue as a diagnostic tool. I’ve noticed that symptoms seem to get better and worse regularly (although my long-term symptom progress is undeniable) but my tongue has always done a good job of indicating where things are at. I have a very thick yellow coating.
Is there anything you can recommend to me as I am getting ready to start this triple therapy?
It would be unethical for me to make recommendations without knowing a person’s case in detail. I do offer a distance patient program in case you may be interested. Here is the link. Respectfully, Dr. Ettinger
http://www.advancedhealing.com/wp-content/uploads/Distance-Client-Program-revised-08-22-17.pdf
Hi Dr. Ettinger:
Would taking monolaurin for 3-4 weeks make a stool antigen test false? I was self-treating before having the stool test.
Would a breath test be more accurate?
Marc,
It is possible. Even if you take a breath test you would need to wait at least two weeks to allow for any possible bacterial suppression to end. No reason to spend money on a test that may come back with a false negative. No enzymes, PPIs, biofilm, probiotic or antimicrobial supplements.
Respectfully,
Dr. Ettinger
Can one get monolaurin by eating coconut?
Coconut oil and certain coconut products contain approximately 50 percent lauric acid. Monolaurin is many times more effective than lauric acid at killing viruses and bacteria; however, researchers aren’t sure exactly how it’s formed in the human body.
Lauric acid can be ingested in coconut oil and your body will convert it into monolaurin, but researchers are unsure of the conversion rates. Because of this, it’s impossible to say how much coconut oil you would need to ingest to receive a therapeutic dose of monolaurin.
I wanted the biofilm protocol, not showing up when I click on it.
The link seems to be working fine, but here it is anyway. Thank you for the interest. http://www.advancedhealing.com/biofilm-protocol-for-lyme-and-gut-pathogens/
I need help. I have been on 12 different antibiotics and I keep becoming resistant to the anabiotic‘s And it comes back stronger what should I take??
Dana,
If I had a crystal ball I could answer that question.
If you are interested in discovering the reason behind it, I can help you with you becoming a distance patient. If interested I can be reached @ 714 – 639 – 4360
Respectfully,
Dr. Ettinger
Hi Dr Ettinger,
I am on day 12 of natural protocol to get rid of H. Pylori. Felt great within a few days, had herx reaction on day 2, then felt much better, like a miracle! As of last night, I started having reflux like symptoms, burning in back of throat and it has continued into this morning. I have been diagnosed with mild reflux for years, but rarely does it ever cause pain. My question is, have you ever heard of the protocol causing reflux symptoms? Or is it that it’s getting worse before getting better?
Protocol: mastic gum, 2 pills 2x day on empty stomach, monolaurin 2x per day w/food, digestive enzymes after meals, l-glutamine w/breakfast and interfase plus 2 pills, 2x per day away from meals and other supplements, and a good probiotic. Could any of these cause reflux? My 2 doctors I have seen for h pylori think this natural stuff is a waste of time, but I feel better than I have in 7 months, apart from this new symptom of burning in the mouth / reflux pain. Any thoughts?
Is there a certain supplement I need to take less of, that may be contributing to reflux symptoms? Greatly appreciate your reply. I have had so many tests, been to several doctors, etc and been treated once with conventional triple therapy for h pylori, which returned. I just don’t want to stop the protocol to have stomach issues return, because of reflux. Desperate to find out if I need to adjust protocol somehow? Thanks in advance, Steve.
The only product that may cause some issue is the Interfase Plus, because of the EDTA.
Hi.
you mentioned the interface plus for the biofilm. my question is it neccesary to take the plus version with the EDTA that chelate minerals? or the non plus version (without EDTA) will be good as well? cause i read some users reported of minerals deficiency when using the plus version. and i don’t want that
thanks
Amir, I can’t promise you that the EDTA won’t pull excess minerals out. The EDTA in interfase plus is quite small. If others have complained about mineral deficiencies, it’s most likely they were taking it long term, in very high doses or had underlying mineral deficiencies to start. A short course of it (less than 60 days) should not create a problem.
I suspect the failure rate for h pylori drug therapy is significantly higher than reported. I did not do well on quad therapy with flagyl and doxycycline;after four days I was ready to kill myself and hyperventilating. My gastric symptoms worsened to the point that I was constantly crying and anxious. My entire system is now inflamed. And my doctor’s office has yet to help me, because I doubt they believe me or know what to do now.
You touched on several factors that contribute to therapy failures. Mine stems from the combination of being given a drug (doxycycline which I react to) and the fact that I am a rapid metabolizer of first generation PPIs. I am chronically dehydrated despite drinking lots of water, it seems to run right through me.
Because I was so sick I sought emergency room care, despite being terrified of contracting C diff, but unfortunately in this visit there was an incidental finding of an 8mm brain aneurysm. ( too complicated to tell how I ended up with CT scan) I have a follow up appt. to see a neurosurgeon, but I am so sick from h pylori I am not sure how I can manage to go it and be told I must have surgery immediately.
In addition, I have peroneal tendonitis in both feet (swelling, too) and I am on crutches. I just can not seem to heal from this and I believe the h pylori is the root cause, but the medicos I talk to dismiss it as a fancy of mine, yet there is good scientific evidence to support my belief. The orthopedic surgeon wants to give me cortisone shots, but I have delayed hoping to heal on my own, but h pylori may be making this impossible. I am in so much pain I can not think clearly.
Elle, Don’t give up! There is help. http://www.advancedhealing.com/wp-content/uploads/2012/07/Distance-Patient-Program-revised-8-15a.pdf
Hi Dr. Ettinger,
I found your site through Amy’s site and am very grateful for her referencing you.
I am helping a friend – PB – who is not able to connect directly with you because of his extreme weakness. I would appreciate your comments regarding alternative therapies such as Lauracidin (which I personally use and think is wonderful), Mastic Gum, Manaku Tea, Manuka Honey etc. while using the HP-Pac (lansoprazole – clarithromcyin – amoxicillin) which he started 3 days ago.
Paul was diagnosed with H Pylori a year ago. He chose not to take treatment at the time as his symptoms seemed to go away on their own and he had no reoccurring stomach symptoms other than bouts of leg pain and his ongoing meniere’s disease
8 Weeks ago he had a sever “stomach flu” which has caused him to experience increasing stomach difficulties and to become weaker and weaker and weaker. I have been helping him by making organic bone broth, vegetable soups etc and ensuing he is eating gluten, dairy and sugar free and taking probiotics and digestive enzymes.
PD was diagnosed yesterday with H Pylori and has begun HP-Pac – he is having a lot of gas and stomach pains since starting but is drinking a lot of water. He is desperate to get better given his 8 weeks without being able to work.
Can you please comment which alternative treatments you would specifically recommend adding to his current allopathic treatment?
Also, I am very familiar with biofilm from lyme disease and wonder what the tell tail symptoms of H Pylori biofilm are?
Thank you so much for your response.
Andrea
Andrea,
There is a lot going on there and you seem to need a medical assessment on him, which I can’t do in this forum. I can help but the liability of just blindly making recommendations with his advanced condition would be unethical. I do offer a distance patient program which would be perfect for this situation. Please go to the “Forms” section of my website and view my “Distance Patient Application.” If PB is interested, he just needs to follow the instruction.
I wish you both the best.
Respectfully,
Dr. Marcus Ettinger
Dr.Ettinger, Thank you for the comprehensive information you have provided for so many of us who are struggling to regain our health and not having any success using antibiotic treatments. I have subsequently developed gluten and salicylate intolerance since the Gastritis began 3 years ago so my diet is very restricted now and I am probably deficient in zinc amongst other vitamins and minerals. I realize now I was chronically dehydrated for most of my adult life and find that drinking lots of filtered water eases the gastritis considerably.
I wonder how many others ( such as ‘name withheld’) end up with food intolerances due to leaky gut as a result of the damage caused by the infection, making their gastritis worse as they continue to eat foods they have now become sensitive to. I will definately be using your protocol and look forward to feeling better soon. Thanks for caring.
Hello, after being diagnosed with active chronic gastritis and h. pylori I started the antibiotic treatment with biaxin the first 24 hrs giving me watery diahhrea for 4/5 hours and had to stop. The metronizadole I tried later gave me thrush, severe heartburn and esophagitis so bad I started gagging after talking (feeling my throat would close) and now have a permanent lump feeling in my throat. I am trying $$ matula tea, mastic gum and gluten free, dairy free diet with low sugar. Anything else? -they need to get my inflamed throat better since Dr.s want to try the antibioitcs again..
Thank you for your sympathy, Dr. Ettinger. I didn’t mean to make it seem like I didn’t realize the conundrum my situation causes anyone I seek out for help. I’ve been to so many expensive consultations, appointments with that information in hand that went nowhere to fully appreciate the predicament for both parties. I just want to get somewhere further than double-talk. May I contact your office next week with the typed document I compiled with the information you asked about so you can, at your convenience, render an opinion? Or would you prefer I put a synopsis in this online format? I don’t want to encumber your time in any way but I’m one of the few who really have almost nowhere to turn. Thank you for your time especially on a weekend.
Dr. Ettinger,
I’ve read through your H Pylori, Biofilm section, questions and answers, forum posts (elswere), etc. several times in the past few months. I respect your experience with treating H Pylori for yourself and your patients.
Unlike you and the others I’ve seen describe their experiences online, my H Pylori is complicated with SEVERE gastritis. I cannot tolerate acids, even essential fatty acids, coconut oil, its derivatives, alcohol-based tinctures, vitamin drops, apple cider vinegar, kombucha, betaine, animal-based enzymes, etc. all set my intestinal tissue on fire, raise my existing high blood pressure significantly, and land me in need of medical treatment. I think I’m reacting to my own digestive acids because every meal and every hour that passes on the clock during the day makes me sicker. My bowel is so toxic that my BP goes up with every BM and any degree of intestinal “peace” I have is shattered. Every leaky gut formula out on the market has ingredients that make me worse: ginger, MSM, marshmallow root, slippery elm bark. Glutamine and mastic gum are ineffective and DGL makes me feel like I’m going to regurgitate. Probiotics and most other treatments seem to work in reverse on me–exacerbating my symptoms not relieving them. Other online practitioners have led me down the garden path and then dropped me once they finally believed my symptoms are this bad and I couldn’t tolerate their “go-to” solutions.
I’m on this route because I cannot tolerate 95% of standard antibiotics and have had proton pump inhibitors ravage my system (unbeknownst to me for five years) supposedly treating this gastritis but obviously not. Now I have malabsorption, nonexistent Vitamin D, B12, and countless other deficiencies including magnesium. However, treating any of those causes my existing chest wall pain and palpitations to become unbearable. I’m riddled with intestinal gas–cruciferous vegetables (juiced or raw) send me running to urgent medical care due to the burning and pain–now I’ve finally developed significant intestinal bloating and constipation that has doubled my abdominal area and left me more worried and obviously sicker than before.
I say all of this to ask you with all sincerity, have you “coached”, counseled, dealt with people whose conditions are as severe as mine? If not, any suggestion of where to turn will be greatly appreciated even if it is to stay on the ferris wheel of MDs, GI specialists, and ER doctors who have failed me thus far for 2 years. I got my Dx of H Pylori from the lab you like so much last November–months after getting off the PPIs that kept showing me a false negative for H Pylori with my former doctors. Thank you for even reading this.
First-off, I’m sorry to hear how bad-off you are. Second, how do you treat someone who can’t be treated? The only way I could possibly help you is to know, “WHAT CAN YOU INGEST W/O CAUSING SYMPTOMS (foods, liquids, supplements…)?” W/O that I wouldn’t even know where to start.
Dr. Ettinger,
Will you please help me. I am h pylori positive and very, very sick. I just began taking monolaurin, this is my 3rd full day. I’ve been taking 4x300mg, twice daily (1200mg in the morning, 1200mg at night). I am feeling 100x worse since starting. I’m scared this is too high of a dose…what should I back it down to, that will still be effective against h pylori?
Please help. I’ve been rushed to the ER several times already this year while trying to find out what was wrong with me (heart racing/palpitations, weakness, near-fainting). We have racked up thousands in medical bills and for prescription drugs that have not cured me. I’m very sick tonight and very scared. Any advice you can give me on what to do with the dosage would be so appreciated.
Cam,
You can take 300mg’s two times per day and work your way-up from there. Important: Monolaurin by itself is not going to do much in the way of eradicating H. pylori. I know you have spent a lot of cash with no results and I would be pissed too, but to help you we need to do it the right way. If you become a distance patient, filling out all the appropriate paper work, we can schedule a consult and lay-out an exact plan to help you get rid of this. Distance Patient Application
If you would like my help, I’m hear to help you.
Sincerely,
Dr. Ettinger
Hi Dr. Ettinger,
Just to clarify, the Monolaurin seemed to exacerbate my existing symptoms such as anxiety, fogginess, headache but it did help with my eczema and seemed to help my stomach. So I am sure that it was doing something. Perhaps I should start at a smaller dose and work up?
Bonnie
Bonnie,
That would be a good idea. Start at 300mg’s 2x/day and work your way up from there. If you have the 600mg’s, just take one per day and work-up from there.
Dr. Ettinger
Hi Dr. Ettinger,
I have been diagnosed with h. pylori through a stool test by Metametrix. I am currently on mastic gum, propolis, zinc l-carnosine, aloe vera juice and have been on these for almost 2 months with modest improvement. I experience gastritis and have an ulcer, which wakes me up at night when I eat the wrong food. I stray from my diet when my stomach feels better and then I suffer the consequences.
I attempted to add Monolaurin to my regimen but it made me feel worse after a week (at 1200 mg a day). Is it possible to experience die-off from the Monolaurin? Should I add anything else to my regimen to address the biofilms, or should I just try Monolaurin again? I also developed a chronic sinus infection. And do you have any advice for healing ulcers?
Is it possible for you to ship your products to Canada? Thanks.
Bonnie
Bonnie,
It’s possible to experience die-off on Monolaurin. I don’t see it very often but it is possible.
If you have a sinus infection it’s most likely a virus and not a biofilm related issue. Monolaurin does work on virus as well. I use it all the time for various bugs the affect us.
My advice would be to set-up a consult with me so we can lay out a specific plan of action. My protocols are concentrated and only take 4-6 weeks. If you go to my “Forms” section on the top bar of my website, the last form is the Distance Patient Application. It will give you all the data you need to become a distance patient. I do ship to Canada
I look forward to hearing from you.
Dr. Ettinger
I had exact results with taking monolaurin. Worked for the moment, but pylori came back 10 fold with avengance.
Dr. Ettinger:
I have an allergy to coconut in which I have severe stomach cramps. Would I still be able to take monolaurin?
I keep monolaurin on hand for my cats, because it cures cytauxzoanosis (bobcat tick fever), which is often fatal. I give one 300-milligram capsule once an hour for eight doses, emptied out and mixed with water and given with an eyedropper. It kills the protozoan that causes the illness and brings the fever down. I’m so thankful for monolaurin.
But I think I may have been exposed to h. pylori, because I’m having many of the symptoms of it, and I wondered if you know if monolaurin would cause the same stomach cramps that eating coconut does for me. It’s mainly fresh or fresh frozen coconut that caused the symptoms in the past. I haven’t eaten it in many years.
Thank you very much.
Melanie,
I have no idea where this was, I look at my comments all the time and this one just popped-up, and it’s from January.
I do not think monolaurin is made from coconut. I think it’s just a bunch of ingredients mixed-up in a lab. I will find out and post what I come-up with.
Dear Dr. Ettinger,
Your blog about H pylori has been of great help. I have had mild to moderate gastritis (as evidenced by recent endoscopy) for the last one month or so. My biopsy revealed a small number of H pylori organisms but no ulcer or erosion. I was on Zantac (150mg) for about a month and a half before I went for endoscopy. Now my GI doc has recommended triple therapy. My gastritis symptoms have disappeared about 50-60% than earlier. I want to try treating H pylori naturally since I am worried about the side effects of the antibiotic. I have started eating Virgin Coconut oil 2-3 tsp a day for the past 2-3 days and I’m going to order some manuka honey online. Do you recommend any particular brand? Also, are there any side effects of Manuka honey? Is mastic gum safe since I have read some forums where people experienced gastroparesis as a result of taking mastic. Please advise. I am willing to call for consultation since I live on the east coast.
Thanks in advance!
Parag,
EVCO is okay at 2tsp/day as is the Manuka honey and mastic gum. This issue with the three is that they are weak as far as treatments go. I do not carry those products in my practice or make recommendations on them because of their lack of efficacy. The protocol I have put together is very effective and I have pre and post tests to that fact. If someone wants to take the above three in addition, all the better.
I do offer distance patient consultations. The majority of H. pylori patients I help are helped this way. Please follow this link for the data. I can also be reached if you have questions on the distance patient consulting at 714-639-4360
Sincerely,
Dr. Ettinger
Hi Dr. Ettinger,
You mentioned that you went on a pre-treatment with antacids to heal your GERD/Gastritis symptoms before going on the H. Pylori protocol with Interfase Plus, and other supplements. How long would you advise going on antacids before attempting your protocol? I’m afraid to go on prilosec considering it may make my H. Pylori worse; yet, I need to heal from gerd/gastritis symptoms. I believe I may have low stomach acid as well. Any suggestions?
Marie,
I can’t make a recommendation on how long you should take an antacid. The Prilosec will not make the H. pylori worse and is taken during the eradication phase. Most people over the age of 40 have diminished capacity to produce adequate HCl in the stomach. I take a digestive enzyme containing HCl with all of my meals.
I hope this helps.
Dr. Ettinger
I just found your website and I am hoping you can help me. We travel the world as a lifestyle so that complicates things, but we are in California for a few months now.
http://www.soultravelers3.com/2011/09/travel-health-secrets-for-long-term-digital-nomads.html#more
I have had severe digestive problems since last May ( a year and half ago) and a very distended upper stomach since last February when it kicked up into even higher gear. I have gotten relief with acupuncture, TCM herbs and tried many of the products you mention ( but not in your order or all of them).It comes and goes in severity but some swelling and discomfort has been constant, some days or middle of the nights …emergency room level distress.
Can you tell me what your rate of long term success has been with your protocal? I do not want to take the antibiotics ( I have had candida in the past and respond much better to alternative methods) but have wasted a ton of time and money on finding a cure for me, that I am too desperate now to waste any more time. I need success now and am willing to do what that takes.
I spend all day, every day on trying to feel better and still remain up and down, usually more down than up. I need to get out of survival mode. I spend 2 to 3 hours or more every day doing saunas and hot tubs with jets on back ( back of distressed stomach area) between cold pool swims as that usually gives me some relief from the severe toxic feeling. ( Doing this daily since Feb).
I hope you can help me as everyone says the only cure for hpylori is antibiotics, but I am pretty sure the allopath way will make me sicker.
My success with my H. pylori protocol is 100%. That said, it doesn’t mean that if we eliminate the H.pylori your symptoms will disappear. Only if H. pylori is the only factor will you have complete relief when it’s gone. If you are anywhere south of Santa Barbara and North of Baja California, it would be best to come in and see me. You may also call me at 714-639-4360 for distance help. I look forward to hearing from you.
One year after removing Helicobacter, gastritis symptoms return. I suppose I will have to do another Helicobacter test and/or and endoscopy. Gastritis sucks…stomach and chest pain. I have returned to supplements I used last year, I have noted that I have real relief after taking natural butter (ghee maybe is a better option). In zen medicine I have found some basis to this relief on stomach problem with butter
Dr. Ettinger,
Your website, along with Amy King’s, has been so helpful in giving me a natural alternative to getting rid of H. pylori. I’ve been very sick, mostly all undiagnosed by multiple doctors, for over 4 years! I’m hoping being free from H. pylori will help many of my symptoms. I am on a protocol twice a day of 4 different biofilm busters, 4 different anti-bacterials, and a few different “clean-up” methods. Plus, other helpful supplements, probiotics, etc for gut healing.
Two questions:
1) I have Mitral Valve Prolapse and the frightening heart palpitations, light-headedness, difficulty breathing, and low level anxiety that goes along with it. Since starting the protocol it’s getting a lot worse. I fear not taking Magnesium (due to the biofilm) is really taking a toll on my heart. Would it be too detrimental to add it back? Any other recommendation for the MVP while doing the protocol?
2) I’m currently using activated charcoal, apple pectin, psyllium husks, and spirulina for the “clean-up”. I’m concerned (not sure of the long term effects) about taking charcoal daily for 6-8 weeks. Should I be?
Thank you for your time and any advice you may have!
Marcella,
Take the magnesium at least 3-4 hours, before or after, the biofilm “busting” supplements.
I am not a big fan of activated charcoal as a dietary supplement. I would take a heaping tablespoon of the spirulina instead. NAC is a good product too.
Dr. Marcus Ettinger
Dr. E
Can I continue taking the supplements I mentioned earlier right up to when I give my stool test or do I have to quit? With antibiotics I have to wait 2 months before testing. Maria
Maria,
Supplements are fine, as long as they are not anti-parasitic. If you are taking any anti-fungal, bacterial or parasitic medications, you will have to wait.
Dr. E
Hello Dr. Ettinger,
I too have H. pylori (diagnosed last November). I’ve been on two antibiotic treatments, one Prevpak which I didn’t finish and recently Pylera for 10 days. I also have gastritis. I was feeling fine after I finished but the gastritis came back which leads me to believe that I still have the H. pylori. I also lost 28 lbs. I’m down to 100 lbs which I can’t afford to lose. In between the antibiotics I was working with an herbalist here locally. He put me on chlorophyll and a powder of slippery elm, DGL and cuttlefish twice/day. In addition I took mastic gum, Pine nut oil and regular supplements (probiotic, D3, B12, multi etc.). This did not eradicate my H. pylori. He said I had low stomach acid and taking this stuff would heal my stomach lining and the H. pylori would die. In addition to the above I am drinking a lot of cabbage juice and have added oil of oregano to my routine.
I will give another stool test next week and should have the results in two weeks when I see my GI doc first week in Dec. Question – is it possible to have a negative result if I still have gastritis? I’ve been reading all your posts and willing to follow your regiment especially because you went through it. What do you recommend that I haven’t mention above? Do you do private consultation (by phone or email)?
Many thanks.
Maria,
Yes, it is possible to still have gastritis and a negative test. My recommendation is to have a new stool test and then we can rule-in or out H.pylori as the cause. At that point it will be a lot easier to nail-down the cause and handle it. I will forward you a distance patient form. Please get in touch with me when you get your test results.
Dr. E
After 4 months with 2 antibiotics for 7 days I have done now a stomach biopsy and a breath test.
Breath Test: Positive for Helicobacter
Stomach Biopsy: Negative for Helicobacter, not found.
Now I continue to have light stomach pain only after lunch and another 3 weeks before new consult with my new physician. Very confused and dissapointed with my situation after months 🙁
I suppose biopsy is more reliable than breath test.
Hi Dr. Ettinger:
Your website has been very informative! I’ve enjoyed reading about your experiences and advice! I also have H. pylori and have been battling this nasty bug for many years off and on. I took Prev-Pac in January only to find out recently that I’m still positive. This time my gastroenterologist prescribed Pylera but after reading all the serious side effects, especially with the CNS I’ve decided to try the alternative treatment. I’m not willing to take a chance on Peripheral neuropathy, tingling in arms/legs and the worse one convulsive seizures! I just started taking Monolaurin but after reading that it has Isodine in it, I have stopped. I am allergic to Iodine and I wasn’t sure if it’s the same as Iodine. I will buy Monolaurin without the Isodine. I’m also taking the Manuka Honey, Garden of Life Ultra Probiotics. I have Diabetes II and have maintained it for several years with taking Glucophage and watching the diet. The last couple of days I did not take the Glucophage thinking the diet with no sugar, white flour, pasta’s, etc. my B.S. would be O.K. This morning after taking the Manuka honey and Probiotics I took my B.S. and it had spiked to 280. Can these products cause the B.S. to go high? Since I just started this regimen I’m still learning about these products. Any help you could advise would be greatly appreciated! Thank you.
Marcia,
Sorry for the late reply. For some reason this slipped through the cracks. First, check your bottle and see it the ingredient is “Inosine.” The brand that I sell is by Ecological Formulas and is 600mg’s Monolaurin and 7.5mg’s Inosine. Inosine has been shown to exert potent effects on the immune, neural, and cardiovascular systems. I don’t think the ingredient is Isodine.
Manuka Honey will definitely raise your blood sugar! I treat a ton of pre-diabetic and diabetic patients. The key to reversing it is to avoid ALL sugar sources, including starches. That means no: milk, bread, corn, pasta, potato, cooked carrots, rice, oatmeal….
I have had H. pylori for over a year now. I have been on two courses of antibiotics. I just started the tea. Very apprehensive . I really don’t know what to take . I’m changing my diet trying to eliminate gluten and dairy. Please help. What really works.
I need to add that I took a lot of antibiotics in my life since i use to suffer from sinus infections. I am also suffering from anxiety which has to be related to the H. pylori as both started at the same time. I started taking tranquility from Steiner (Don Quay) and it helps with the anxiety. The anxiety comes and goes.
Thanks Gloria
Gloria,
It is very important that you read all my posts on biofilm (Biofilm Protocol). This is the reason why infections (sinus, gut…) go chronic and why antibiotics are not effective in getting rid of them. A gluten free diet will help make everything you do healing-wise, easier. I like moderate exercise for stress relief. Anxiety is a result of when you feel that things are out of your control. Get educated on biofilm, surround yourself with supportive people, eat a natural diet and get in regular sleep and exercise. I hope this is of some help to you. Please update me on how thing go.
Sincerely,
Dr. E
Thanks for the e-mail, I understand your situation. I was reading your biofilm protocol and you mentioned seeing big differences around day 66. Can you go into a little more detail on what you saw around that time? Thanks
I see, so Klaire Labs – InterFase Plus, 2 caps 3x/day on an empty , is what I should I take? Do you recommend anything else to take along side with this? Should I still take the monolaurin and the Herbal anti-bacterial?
Thanks, when you say bacteria, are you referring to H pylori? Should I start the h pylori regimen you mention above in the post?
It’s not H.pylori. The biofilm protocol will help to breakdown the protective coating that has protected the bacteria from being killed by antibiotics or your own immune system. I have no idea how long it will take but it’s the best treatment advise I can give you.
BACTERIAL BIOFILMS IN SURGICAL SPECIMENS OF PATIENTS WITH CHRONIC RHINOSINUSITIS (sinusitis).
Sanclement JA, Webster P, Thomas J, Ramadan HH. Department of Otolaryngology, West Virginia University, Morgantown, West Virginia 26506-9200, USA.
CONCLUSIONS: Biofilms were demonstrated to be present in 80% the 30 patients undergoing surgery for chronic rhinosinusitis (CRS); none of the (control) patients without CRS had any evidence of biofilms.
Last year I read someone’s blog/abstract about biofilms and it was so scientific and overwhelming, I glazed over and kept driving. Yesterday I was trying to figure out why I could not handle the oxalates in this new green juice I’ve been making that my body seems to have a love/hate relationship with (parsley, celery, cilantro, unheated honey, green papaya, vco). All roads pointed to biofilms.
I have to pinch myself that I found your website and blog. I’m 42 and carry an extra 50lbs. I have been dealing with weight and gut issues for many years; ACL replacement in Oct. ’02 at which time I took 2-3 800mg ibuprofen and (several) vodka tonics every day until Jan. ’05 when I got pregnant. My health was not good during the pregnancy and it is a wonder I didn’t give birth to a GMO alien. For the last two years, I have been really serious about healing. In ’08 we started with a Weston Price type lifestyle and I thought this would cure whatever was going on with my gut.
Earlier this year I saw a Chiro/ND who did Kinesiology and had me taking all kinds of supplements (my stomach could not process/utilize). The HCL he gave made me double over in pain. He said there was no H. pylori. That was difficult to believe when I found and started taking mastic gum and started feeling a whole lot better. If it’s not H. pylori, it’s something else causing inflammation/ulcers because the green juice set it off. I thought I had found the missing link with mastic gum. I was/am already on to zinc, Ulcetrol, dgl licorice, coconut oil and anything fermenty and drinkable I could get my hands on. Now’s Plant Enzymes with a big spoonful of coconut oil feels pretty good.
It seems now, that biofilm (and fixing it) is the missing link and I intend to implement your full regime. I wish I had another $270 to get formal testing and a good crack. I see that if I drive to your office, I can stop at Desert Hot Springs and take a soak – is it true there are trace amounts of lithium on those springs?
Speaking of which, dead sea salt has been my best friend lately – I thought my guts for sure would heal with soaking in dds and doing the awesome new green juice (Aajonus recipe). Maybe that can be my woobie for when this is all over. Biofilm seems to build its network using magnesium, iron and calcium. Unfortunate.
The only thing I’m somewhat concerned about with the EDTA is the herxing/detox. I take livery stuff, but not really anything for kidneys.
Thank you so much for providing this information, making all these things available and accounting what you did for your own guts. Mucho gracias!
Vanessa in Tucson, AZ
About six months ago I started feeling weak in the morning and very anxious. Recently I was diagnosed with H. pylori bacteria and was put on triple regimen (amoxicillin, clarithromycin,and lansoprazole). I, however have no pain only burping and flatulence. I have no appetite in the morning but it comes on in the evening. Now I feel weak in the morning after taking the tablets but okay at night after taking them. I have ordered pine nut oil. Should I stop the triple regimen and use only the oil or use all four to get me feeling better
I would continue on the triple regimen and the oil. Now is the time to add a potent probiotic like GR8 or Probiotic Defense Powder. Both by Now Foods. I would also add some vitamin C and extra fiber to your daily program.
Get retested with a stool test around 30 days post antibiotic therapy.
Dr. Ettinger, my father, 70 yrs old, generally of good health, was diagnosed with H. pylori last November. He has had three treatments with antibiotics without results. The level of the bacteria remains high, although he can eat without getting sick and has no stomach pains. We started looking for alternative remedies. Nine days ago he implemented a new diet consisting of fresh raw garlic, lemon grass tea, ginger, oregano, & curry. Only eats fish and chicken for meat. We also found lemon grass oil and ordered it, however it has not yet arrived. We had read an article about scientific research in Kyoto Japan that says H. pylori did not build resistance, even after ten sequential passages using mice.
We need someone to tell us what to do.
Can you make any recommendations?
By the way, he lives in Panama Central America, and we understand the strands vary significantly by regions.
Thank You.
Ramon,
Please read my post on H. pylori treatment. The post contains the information needed to make an informed decision on which products to use and why H. pylori is so hard to treat. Minimally your day needs a potent probiotic.
Thanks so much for your reply. I am allergic to dairy including casein. Would I react badly to L. Casei in a probotic. Finally, my gasto doctor just prescribed Refaximin to kill of the E Coli. I took it for two days and got very constipated. Have you heard of using Refaximin (Xifaxan) to treat those with dysbiosis that causes constipation? Thanks for your reply.
Debby,
All probiotic bacteria are perfectly safe! E. coli is a normal constituent of our intestinal tract and should not be treated as a pathogen. E. coli induced food poisoning is acute and is a totally different issue. Just my opinion – stop the antibiotics.
Now is the time to get on a high dose of probiotics, fiber and a healing agent like Ulcetrol.
Dr. E
Dr. Ettinger, I have had these symptoms for probably over 10 years now. I also have constant nasal congestion, white coating on tongue, and constant bad breath. I have seen my regular physician and tried many different medications however nothing has helped even 1%. I saw an ENT about 2 years ago and got sinus surgery done as he said I had a deviated septum. The surgery did absolutely nothing and I still have the same symptoms to date. I have never seen a GI or got tested for H pylori, but I believe this may be the cause of all my symptoms. I was recently tested for parasites, and it came back clean. Where should I start? Please help.
Chris,
The reason that nasal symptoms haven’t cleared-up is because the bacteria are encased in a biofilm. Please read my posts on biofilm and you will finally have the answers to your questions. If you need to order the biofilm protocol nutrients, please call our office 714.639.4360
Biofilm Basics
Quorum Sensing and Biofilm
Biofilm Protocol
Hi, Dr. Ettinger, a few questions about your protocol before I start. I’m assuming that the treatment period is 8 weeks? Also do you have to remove certain foods like dairy, gluten, sugar when on this. (Remove known allergens?) Thank you
John,
The protocol, on average, is eight weeks. Yes, I would eliminate gluten, dairy and tomato based products.
I have been sick since January 31. Stool test showed no H. pylori but a dysbiosis that includes E coli. Since I had a colonoscopy in April, gastritis has gotten worse. I have been taking Natren’s Healthy Trinity… and stools have become regular, but gastritis worse. I lost weight and have trouble keeping it on, nervousness and anxiety. I have been told that Mastic Gum can kill bacteria other than H. pylori that may be the cause of my digestive disorder. I noticed you have shown there that the coconut oil doesn’t kill E coli.
Any suggestions for me?
Thanks
Debby,
Try Ulcetrol (1/3x day – has mastic gum in it) and GR8 1/2x day – probiotic formula). Both are from Now Foods and can be found online or in most good health food stores. Without knowing more about you it is had to give more recommendations. This is a good start.
Hi again. I started 4-5 weeks ago with Source Naturals Mastic Gum (2/day), coconut oil, Source Naturals broccoli extract (3/day), different probiotics (2/day), zinc-carnosine with DGL (2/day), some of manuka honey, quercetin (250mg a day), Pure-Way C (500mg 2 per day), siberian pine nut oil (1 spoon per day), aloe vera and InterFase Plus, then I added origanum oil 4 drops a day and HPLR from Apex.. 4th week I improved so much that I felt as almost healed, but 5th week my stomach pain returned, not so strong like in the beginning but I felt bad again. Now I have added Broccolive from New Chapter and Fungal Defense from Garden of Life.
Few days ago I went again to my doctor and I will be under a endoscopy next July 1st to check out current state of my stomach and to discard any other possible problem like any kind of ulcer, hiatal hernia.. (but its impossible my pain come from a hernia because I feel pain even fasting when I wake up and typical treatment for hiatal hernia, Omeprazole, doesnt solve me anything).
If Helicobacter persists in next weeks most probably I will have to be under a new round of antibiotics.
Is curious. Yesterday I finished 7 days of antibiotics and place of my pain has changed in these day: before in lower esophagus and top stomach and in last week and now only in lower stomach.
I cant find on internet InterFase for european customers. I will try monolaurin. I feel I will have to be done an endoscopy (Helicobacter was detected with blood and breath 15 days ago after 1 month of pain).
I have read there are some positive studies about lemongrass oil against Helicobacter but I consider it too strong for my sensitive stomach now :S
David,
“The current guidelines suggest the use of triple therapy as first choice treatment of Helicobacter pylori infection, although the eradication failure rate is more than 30%.” Department of Paediatrics, University of Catania, Catania, Italy – April 2010
H. pylori is more effectively treated, in my opinion, naturally. You may want to get retested to make sure it is gone. Stool testing is my preference.
Since you have these products available, get started on them. Probiotic (1 3x/day), vitamin C Pure-way (1,000mg’s per day), aloe vera (if juice – 1 oz. 3x/day), zinc-carnosine formula (1 3x/day) and broccoli extract 1 3x/day). This will aid in the healing of the membranes in the GI tract.
Let me know the results of the follow-up testing.
Thanks for this information Dr Marcus. My mother and me have helicobacter, after 7 days of antibiotics abdominal pain goes on. Yet no new test of helicobacter, we suppose it has not gone. We are trying natural approaches with mastica gum, manuka, 2 probiotics, vitamin C Pure-way, aloe vera, zinc-carnosine formula, broccoli extract, origanum oil and maybe also siberian pine nut oil. We already consume Omega3 and vitamin D3 time ago.There is a tea called Matula but I think its not serious. Thanks from Spain
Do you still recommend the antacid for pretreatment? Is there a natural version of that? Plus, it seems the opposite of the HCL I take in order to get anywhere with digesting food. Am I understanding correctly? So would you recommend no HCL and antacids for pretreatment? And for how long?
By the way, I am doing the Gut and Psychology Protocol (GAPS) and it has been very helpful and a great way to heal the digestive tract – but I need to get rid of both H pylori and klebsiella pneumonia. I really appreciate your clear protocol for treatment. Thank you.
Elli, you are correct, no HCl during the killing phase. A generic antacid is fine. There isn’t a natural alternative. As long as you are trying to kill the H. pylori you will want to keep the HCl to a minimum.
Make sure you are using the Monolaurin and the InterFase Plus. Biofilm is the main reason chronic infections don’t resolve. You have to remove them to get to the infection.
Hi Dr. Ettinger, I had a consult with you about 8 weeks ago, and at the time I had severe stomach pain, sleeplessness, weight loss, depression/anxiety problems. Since then, I have progressively been getting better. I started a detox elimination diet that has worked wonders, and I am down to trying to wean off the prevacid. My H-pylori stool test came back negative about 1 month ago. I am still having stomach pain, but it is mild compared to before. I am sleeping well and anxiety/depression symptoms are gone. I did find out that I am sensitive to wheat (gluten), and I have some problems with peanuts and maybe soy. I am just wondering what I should do now to heal up my stomach completely and get off the prevacid? Any ideas.
Susie,
That’s great! It sounds like you are doing all the right things. For healing, I like Ulcetrol by Now Foods, a daily probiotic, cabbage juice or eat a lot of cabbage, brussels sprouts and/or broccoli. If you need help with digestion, I like Plant Enzymes by Now Foods. I hope this helps.
Thank You…
Should I add the monolaurin or coconut oil to what i take to help get rid of the h pylori?
Chris,
Coconut oil is 50% lauric acid by volume and Monolaurin is 100% lauric acid. I recommend 2 600mg Monolaurin caps 2x/day, mainly because it is easier. Also, I take 1 tbsp of flax oil and 2 tsp of fish oil per day, and I use a lot of EVOO for cooking and salads. I don’t really want another two tbsp of oil in my diet.
I hope this helps.
So what exactly should I take it seems like ur adding a bunch of different things. I started to eat broccoli sprouts right now to, maybe it will help and im taking the candicin. Would adding coconut oil be just as good as the monolaurin?
Also the biggest problem to is that i lost so much weight. I used to weigh around 180 and now im down to 146 and i cant seem to go up in weight. I can’t seem to figure out why. Would H pylori make you lose that much weight?
Chris,
I am sure you can appreciate this, It’s almost impossible for me to give you competent advise without seeing you and having test results and a in-depth consultation.
There is definitely a GI problem still, we both know that. As an experiment, I would try 2 tbs of psyllium fiber, 1/4 tsp Now Foods Probiotic Defense Powder (to start), mixed in yogurt and 1 Now Foods GR8 capsule. This should be done 2x/day. Call if you want to buy these – 714-639-4360.
This will normalize the environment of the GI tract. Let’s see what gets better and what stays the same. By ruling things out or in, you will be better able to figure out what is the primary cause(s).
I have h-pylori and it has been making me feel awful. I feel bloated all the time, heartburn and just feel week. My potassium has dropped to 3.5 from 4.5. A naturopath put me on candicin which has oregano oil and wormwood, ginger and clove oils. She also told me to take bee propolis cuz it will help. I started to think that I need to take antibiotics cuz I am not feeling any better. I’m wondering if you can help me on what to take or if what i am taking is good enough. Thanx
Chris,
I have never used that combination of products before to kill H. pylori, so I really can’t say if it will or won’t handle it. I do know that the combo is good for candida and parasites. Personally, I would switch courses and go for a tried-and-true protocol, like the one listed on my H. pylori blog post. Antibiotics may just make things worse for you. Meaning, it may kill the H. pylori but cause all kinds of GI side effects (most antibiotics do). So, you are H. pylori free but now have a raging candida over-growth, depleted beneficial gut bacteria and generalized irritation to the stomach and intestines.
I hope this is of some help.
Dr. E
Dear Dr. E,
Firstly, thank you for your H. pylori info – about the most informative site I have seen. I think I have H. pylori. No pain or discomfort, but a lot of burping. I took mastic gum religiously for a month – the Solaray one – it said on the bottle you had to take it for 28 days to cure H. pylori – after that you take a maintenance dose. I’ve been a bit lax with the maintenance dose though. One problem is that I feel very tired. Is this the mastic gum or the H. pylori causing tiredness? I am so, so tired, it’s affecting my life. It’s awful. I have heard that some of these natural remedies – like Siberian pine nut oil which is also supposed to kill H. pylori too – have detoxing effects which include tiredness. What is one to do? Does monolaurin also cause fatigue? I am thinking of trying it because I have started burping again.
Linda,
Mastic gum, monolaurin or the pine nut oil shout NOT cause you any tiredness or detox type reactions. If the burping has come back it can be do to many factors. The H. pylori may not be gone, your food combining may be causing the gas, there may not be enough friendly bacteria in the gut, and or you may have candida.
The monolaurin combined with Ulcetrol from Now Foods and a potent probiotic, like Probiotic Defense, also from Now foods, should do the trick. Just to hedge your bets, you may also want to add a plant based digestive enzyme. I like Plant Enzymes for Now Foods – 1-2 with each meal.
If you need any help getting these products give us call us at 714-639-4360 and we can get them right out to you.
Thank you. Glad to know there is hope in dealing with this! I have gradually lost 20 lbs of weight from this infection!
Quickly, would you recommend one to get on HCl pills and probiotics once we test negative?
I have heard mixed reviews about bottled probiotics. Some claiming they are dead even before they hit your front door. Can I get your 2 cents on this Dr.
Ryan
Ryan,
I like Super Enzymes from Now Foods. It is a great digestive enzyme with HCl and is something I recommend after H. pylori has been handled. Probiotics from reputable companies are very stable. I like GR8 from Now Food. I have used it for years with great success.
Let me know if you need any help getting these products.
Doctor Ettinger,
Hello. How is your gut doing since treating H. pylori?
do you or any of your patients have experience with Manuka honey?
Thanks and Best of health to you
Ryan
Ryan,
My stomach and digestive tract is 100% back to normal. I have not recommended Manuka honey. Not because it’s not good for you or that it wont’ help, its just that their are better, more effective products out there.
Dr. E
Thanks for the quick response. As far as mastic gum goes, are
you still prescribing it for “healing” purposes, as opposed to treating
pylori?
I’ve been on a regimen of aloe vera juice, cabbage juice, slippery elm and
mastic gum (2 grams a day) for the past month and have progressed
a lot. Is this too simplistic for you?
Dr. Ettinger,
what brand of Monolaurin do you recommend for pylori patients?
Ecological Formulas 600mg caps – 2/2x/day. 2,000mg’s is a daily therapeutic dose, more is not better.
Hi again Dr.E, I have redone my urea breath test for HP at the end of January ’10 and it came negative! voila!
Hi Dr. Ettinger,
I also have been to Amy’s website have found a lot of great info there. I was scared with the heart palpitations and the immense pain I felt in my side and back. It has subsided greatly since I have started with the monolaurin, mastic gum and Manuka honey, probiotic VSL#3. I did start off with the triple antibiotic treatment from my doctor back in November, but to no avail. My question is when I stopped the triple antibiotics I have had a pain in my very lower back or upper buttock region that I can’t explain, almost like it is my tailbone but not quite. It has been there since I finished the antibiotics and also my left heel has tremendous pain in it sometimes(most of the time) when I walk on it, so therefore I limp. Did not have this before antibiotic treatment. Could the h-pylori have anything to do with this?? I have only been on the natural treatments for a week now and I am hoping to feel better in a few months. Also should I take the H-PLR with the rest of the stuff I am taking?? Thanks so very much for any help you can offer me.
Patty,
Were you on: Cipro, Avelox, Proquin XR or Levaquin? As these can all cause spontaneous Achilles tendon rupture or Achilles tendonitis.
H-PLR with the rest of your supplements is perfect.
I was diagnosed with Helicobacter pylori (H. pylori) in May.09, but I’ve been having problems for much longer that that. This bacterial situation has actually been on and off for several years, but in 2009 it got much worse. It got so bad that I wasn’t able to do a urea breath test, because I couldn’t stand without the proton pump inhibitor (acid blocker), Losec, in my case. So I had an endoscopy to be diagnosed with H. pylori. As a first round therapy I had the standard "triple therapy" (2 antibiotics and one antacid). In May I first tested positive, again in July, and again in August, so this time I was put on "quadruple therapy." I finished that up and after just one week off the drugs all my symptoms came back. My biggest symptom was lots of heartburn, really bad. I was having heartburn from everything, even from plain water.
Seeing that antibiotics didn’t help, I decided to look for help on the internet. I found different forums where people were sharing same stories as mine. Than I found Matula tea: I bought one month supply, 150$ US dollars (I’m in Canada). The tea helped for exactly one moth and after that my
symptoms came back. I never gave up, I looked again for help; this time I found Amy King’s blog, sending a link towards Doctor Ettinger’s website. There I found his story; he actually, himself, had H. pylori at one time, and shared his experience of how he treated it. I decided to follow his protocol step by step.
This was happening in November 09. After 2 weeks of Monolaurin + H-PLR + Enzymes, I was felling better. I had to give up on the H-PLR, as I wasn’t feeling to well from that. Dr. E said maybe it was to strong for me. I replaced it with Mastic Gum. I finished 2 moths of treatment to kill the bacteria and now I’m following
the maintenance treatment. By now it feels so good not to have heartburn, it’s almost gone.
Now what you have to remember is that besides treatment you have to change your life style, what you eat and how you exercise. Exercise with more cardio than weights. About food, try to avoid all foods which will cause you heartburn like oranges, tomatoes, pasta, all greasy stuff and junk food. I
bought a juice maker. During my killing treatment I was juicing everyday: 3 carrots + piece of cabbage + one raw potato which will make you 500ml glass of juice. Even now, every other 3rd day I drink that. You have to make your body more alkaline than acidic. Dr. Ettinger assisted me through this phase, answered any questions I had and supplied me with all of the products. Now I’m felling normal again.
Thank you, Dr. E.
Hi Dr. Ettinger,
I have a really complex issue and was wondering (based on your article) if you could offer me any help in any way. I do not live in your area. I saw that you posted on Amy’s website about H Pylori and was hoping you could offer me your insight just the same.
I had the flu about 12-13 weeks ago. I was in bed and really really sick. During the flu, I took antibiotics (azithromycin). While sick with the flu, I developed upper left abdominal pain. Post-flu I just wasn’t the same. I was worn out, having memory lapse, was so fatigued and emotionally off. I soon developed bad acid reflux, burning in my chest and then anxiety. I did not know what was wrong with me. I was so nauseous, could barely eat anything and developed increasing pain in my upper abdomen. I was so bloated, burping, flatulence, etc. I felt like I just was missing something I had previously.
From there, a whole cascade of symptoms popped up. I was prescribed another antibiotic due to chest congestion and residual issues post flu. Other symptoms I had were a racing pulse, panic/anxiety, burning/stinging skin, spasms in various places, bizarre head sensations (pressure in my head/ears) or tingling, shortness of breath, extreme thirst (sometimes), unintended weight loss, etc. I started becoming increasingly reactive to food- with pressure in my head, shortness of breath, a coating in my throat, racing heart, burning skin, hive-like feelings all over, etc. I am now consuming only organic eggs, organic chicken and asparagus. I was eating apples but had an intense reaction to those yesterday.
I am only 23 years old. I do not have any health conditions (but an obvious issue right now). I have had blood work done and all thyroid, endocrine, blood counts, infectious disease and such come back normal. I have also had extensive tests – ultrasound, MRI and these were okay. My blood work test for H. Pylori came back elevated and it was in the past too.
I am reactive to even supplements. I was on Ultra Flora and became reactive to it after a period of about 5 days. I actually tolerated this the best of most other things. B vitamins have caused my heart to race, magnesium caused extreme shortness of breath, mineral supplements and others have turned my nose and chest bright red with again shortness of breath. Others cause pressure in my head.
I know that I cannot resort to the conventional medical community. I have tried. They don’t recognize leaky gut and such things. I have recently been prescribed even more antibiotics for H. Pylori.
I get really disoriented (especially at night). I sometimes see strips of light in front of my face. My surrounding environment looks like a movie– my perception is distorted- hard to describe. It doesn’t look blurry but rather just different- like a movie’s view of the world and not real life (fast movement for example or different depth perception). I have been told that gut toxins and such can migrate to my brain. Also, deficiencies do not help.
I am really confused as to how to help myself. I know that I am in need of nutrients very much so. I have tried to take Metagenics medical food and even react to this. I need to provide my body with what it needs.
I know this seems so extreme and it is. I have had cold laser therapy and been desensitized to minimize these reactions. I have been tested kinetically to determine what my body needs. I then react to taking what it is needing.
If you can make any suggestions whatsoever, I would be ever so so grateful.
I am not sure how much H. Pylori can contribute to this? I know with some people it doesn’t cause near as many issues as it does others. I also have not read of it causing such extreme food intolerance and cognitive effects, etc.
I know that with all of this, I do not need H. Pylori. I am not sure how to go about eliminating it with all of these sensitivities. Have you heard of H. Pylori causing such things? Can it? Can it contribute to a leaky gut? I am aware of candida and replenishing natural flora. Can H. Pylori cause such symptoms and food reactions?
I know that I need Probiotics very much so. I reacted to what I was taking, so am not sure what else to do. I have so many Probiotics- Xymogen, Ultra Flora, Flora Plus, etc, etc.
Please any insight would be most appreciated. I am trying so hard.
-Mary
Mary, I hope you’re doing better. I see this is a 12 year old post.
I had most of those strange symptoms too. When I try to attack the pylori with monolaurin and such, it attacks back hard.
A green salad with plain chicken pieces and minimal dressing helps
I took Mastic Gum and it killed the H.pylori. I have proof that the test was positive and two months of taking Mastic Gum and the test was negative. So, I do believe it kills the H.pylori, if not why would a medical test show it negative?
Sharon,
That’s great that it handled your H. pylori. In your case it was all you needed, in others it’s not. Maybe you had a mild case, maybe it was just the right thing for your body, maybe you had the bacteria for just a short time and it needed a mild treatment. Regardless I am glad it’s gone.
Now that it’s gone, it’s time to start on a broad spectrum probiotic and HCl to keep it from returning. Thank you for the comment.
Are you still practicing and treating hylori? Are you still taking patients via teleconferencing?
Lorena,
Yes. I’m still seeing patients, in the office, on the phone, and via Zoom.
Dr. Ettinger