Aplastic Anemia
Definition
Aplastic anemia is a disorder in which the bone marrow greatly decreases or stops production of blood cells.
Description
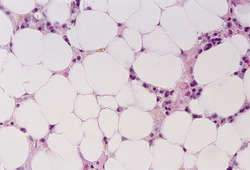
The bone marrow (soft tissue that is located within the hard outer shell of the bones) is responsible for the production of all types of blood cells. The mature forms of these cells include red blood cells, which carry oxygen throughout the body; white blood cells, which fight infection; and platelets, which are involved in clotting. In aplastic anemia, the basic structure of the marrow becomes abnormal, and those cells responsible for generating blood cells (hematopoietic cells) are greatly decreased in number or absent. These hematopoietic cells are replaced by large quantities of fat.
Yearly, aplastic anemia strikes about 5-10 people in every one million. Although aplastic anemia strikes both males and females of all ages, there are two age groups that have an increased risk. Both young adults (between 15-30 years of age) and the elderly (over the age of 60) have higher rates of aplastic anemia than the general population. While the disorder occurs worldwide, young adults in Asia have a higher disease rate than do populations in North America and Europe.
Causes and symptoms
Aplastic anemia falls into three basic categories, based on the origin of its cause: idiopathic, acquired, and hereditary.
In about 60% of cases, aplastic anemia is considered to be idiopathic, meaning that the cause of the disorder is unknown.
Acquired aplastic anemia refers to those cases where certain environmental factors and physical conditions seem to be associated with development of the disease. Acquired aplastic anemia can be associated with:
- exposure to drugs, especially anti-cancer agents, antibiotics, anti-inflammatory agents, seizure medications, and antithyroid drugs (drugs given to stop the functioning of an overactive thyroid)
- exposure to radiation
- chemical exposure (especially to the organic solvent benzene and certain insecticides)
- infection with certain viruses (especially those causing viral hepatitis, as well as Epstein-Barr virus, parvovirus, and HIV, the virus that can cause AIDS)
- pregnancy
- certain other disorders, including a disease called paroxysmal nocturnal hemoglobinuria, an autoimmune reaction called graft-vs-host disease (which occurs when the body's immune system attacks and destroys the body's own cells), and certain connective tissue diseases
Hereditary aplastic anemia is relatively rare, but occurs in Fanconi's anemia, Shwachman-Diamond syndrome, and dyskeratosis congenita.
Symptoms of aplastic anemia tend to be those of other
anemias, including
fatigue, weakness, tiny reddish-purple marks (petechiae) on the skin (evidence of pinpoint hemorrhages into the skin), evidence of abnormal bruising, and bleeding from the gums, nose, intestine, or vagina. The patient is likely to appear pale. If the anemia progresses, decreased oxygen circulating in the blood may lead to an increase in heart rate and the sudden appearance of a new heart murmur.
Diagnosis
The
blood count in aplastic anemia will reveal low numbers of all formed blood cells. Red blood cells will appear normal in size and coloration, but greatly decreased in number. Cells called reticulocytes (very young red blood cells, which are usually produced in great numbers by the bone marrow in order to compensate for a severe anemia) will be very low in number. Platelets and white blood cells will also be decreased in number, though normal in structure.
A sample of the patient's bone marrow will need to be removed by needle (usually from the hip bone) and examined under a microscope. If aplastic anemia is present, this examination will reveal very few or no hematopoietic cells, and replacement with fat.
Treatment
The first step in the treatment of aplastic anemia involves discontinuing exposure to any substance that may be causing the disorder. Although it would seem that blood transfusions would be helpful in this disease, in fact, they only serve as a temporary help, and may complicate future attempts at
bone marrow transplantation.
Key terms
Bone marrow — A substance found in the cavities of bones, especially the long bones and the sternum (breast bone). The bone marrow contains those cells that are responsible for the production of the blood cells (red blood cells, white blood cells, and platelets).
Bone marrow transplant — A procedure in which a quantity of bone marrow is extracted through a needle from a donor, and then passed into a patient to replace the patient's diseased or absent bone marrow.
Hematopoietic cells — Those cells that are lodged within the bone marrow, and which are responsible for producing the cells which circulate in the blood (red blood cells, white blood cells, and platelets).
The most successful treatment for aplastic anemia is bone marrow transplantation. To do this, a marrow donor (often a sibling) must be identified. There are a number of tissue markers that must be examined to determine whether a bone marrow donation is likely to be compatible with the patient's immune system. Compatibility is necessary to avoid complications, including the destruction of the donor marrow by the patient's own immune system.
Patients who cannot undergo bone marrow transplant can be treated with a number of agents, including antithymocyte globulin (ATG), cyclophosphamide, steroids, and cyclosporine. These agents all have the potential to cause a number of troublesome side-effects and may have a success rate of only 60% to 80%. Still, even among those patients who have a good response, many later suffer a relapse (return) of aplastic anemia. Researchers are trying to identify the molecules in certain stem cells that the immune system targets in aplastic anemia.
Prognosis
Aplastic anemia is a life-threatening illness. Without treatment, it will almost surely progress to
death. Survival depends on how severe the disease is at diagnosis, which type of treatment a patient is eligible for, and what kind of response their body has to that treatment. The worst-prognosis type of aplastic anemia is one associated with very low numbers of a particular type of white blood cell. These patients have a high chance of dying from overwhelming bacterial infections. In fact, 80% of all patients treated with blood transfusions alone die within 18 months to two years. Patients who undergo bone marrow transplantation have a 60-90% chance of being cured of the disease.
Resources
Periodicals
Marsh, Judith C.W., Edward C. Gordon-Smith. "Insights Into the Autoimmune Nature of Aplastic Anemia." The Lancet (July 24, 2004): 308.
Organizations
Aplastic Anemia Foundation of America. P.O. Box 613, Annapolis, MD 21404. (800) 747-2820. http://www.aplastic.org.
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
anemia
[ah-ne´me-ah] a condition in which there is reduced delivery of oxygen to the tissues; it is not actually a disease but rather a symptom of any of numerous different disorders and other conditions. The World Health Organization has defined anemia as a
hemoglobin concentration below 7.5 mmol/L (12 g/dL) in women and below 8.1 mmol/L (13 g/dL) in men.
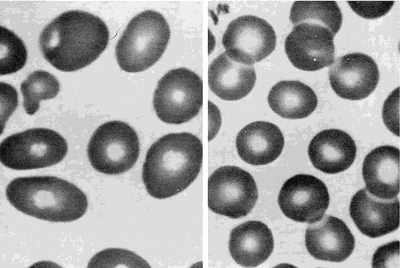
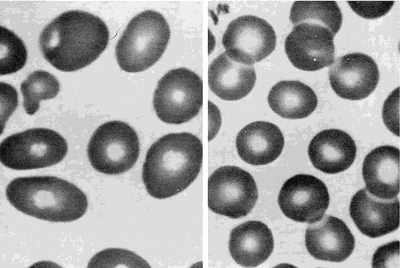
Peripheral blood smears from a patient with megaloblastic anemia (left) and from a normal subject (right), both at the same magnification. The smear from the patient shows variation in the size and shape of erythrocytes and the presence of macro-ovalocytes. From Goldman and Bennett, 2000.
Some types of anemia are named for the factors causing them: poor diet (
nutritional anemia), excessive blood loss (
hemorrhagic anemia), congenital defects of hemoglobin (
hypochromic anemia), exposure to industrial poisons, diseases of the bone marrow (
aplastic anemia and
hypoplastic anemia), or any other disorder that upsets the balance between blood loss through bleeding or destruction of blood cells and production of blood cells. Anemias can also be classified according to the morphologic characteristics of the erythrocytes, such as size (
microcytic,
macrocytic, and
normocytic anemias) and color or hemoglobin concentration (
hypochromic anemia). A type called
hypochromic microcytic anemia is characterized by very small erythrocytes that have low hemoglobin concentration and hence poor coloration. Data used to identify anemia types include the erythrocyte indices: (1) mean corpuscular volume (MCV), the average erythrocyte volume; (2) mean corpuscular hemoglobin (MCH), the average amount of hemoglobin per erythrocyte; and (3) mean corpuscular hemoglobin concentration (MCHC), the average concentration of hemoglobin in erythrocytes. adj.,
adj ane´mic.
Symptoms. Mild degrees of anemia often cause only slight and vague symptoms, perhaps nothing more than easy fatigue or a lack of energy. As the condition progresses, more severe symptoms may be experienced, such as shortness of breath, pounding of the heart, and a rapid pulse; these are caused by the inability of anemic blood to supply the body tissues with enough oxygen. Pallor, particularly in the palms of the hands, the fingernails, and the conjunctiva (the lining of the eyelids), may also indicate anemia. In very advanced cases, swelling of the ankles and other evidence of heart failure may appear.
Common Causes of Anemia.
Loss of Blood (Hemorrhagic Anemia): If there is massive bleeding from a wound or other lesion, the body may lose enough blood to cause severe and acute anemia, which is often accompanied by shock. Immediate transfusions are generally required to replace the lost blood. Chronic blood loss, such as excessive menstrual flow, or slow loss of blood from an ulcer or cancer of the gastrointestinal tract, may also lead to anemia. These anemias disappear when the cause has been found and corrected. To help the blood replenish itself, the health care provider may prescribe medicines containing iron, which is necessary to build hemoglobin, and foods with high iron content, such as kidney and navy beans, liver, spinach, and whole wheat bread.
Dietary Deficiencies and Abnormalities of Red Blood Cell Production (Nutritional Anemia, Aplastic Anemia, and Hypoplastic Anemia): Anemia may develop if the diet does not provide enough iron, protein, vitamin B
12, and other vitamins and minerals needed in the production of hemoglobin and the formation of erythrocytes. The combination of poor diet and chronic loss of blood makes for particular susceptibility to severe anemia. Anemias associated with folic acid deficiency are very common.
Excessive Destruction of Red Blood Cells (hemolytic anemia): Anemia may also develop related to
hemolysis due to trauma, chemical agents or medications
(toxic hemolytic anemia), infectious disease, isoimmune hemolytic reactions, autoimmune disorders, and the paroxysmal
hemoglobinurias.
Patient Care. Assessment of patients with some form of anemia will depend to some extent on the specific type of blood dyscrasia presented. In general, these patients do share some common problems requiring special assessment skills and interventions. Anemia can affect many different body systems
(see table). Although pallor of the skin is a sign of anemia, it is not the most reliable sign; many other factors can affect complexion and skin color. Jaundice of the skin and sclera can occur as a result of hemolysis and the release of bilirubin into the blood stream, where it eventually finds its way into the skin and mucous membranes. (See also
jaundice.) Bleeding under the skin and bruises in response to the slightest trauma often are present in anemic and leukemic patients. A bluish tint to the skin (cyanosis) can indicate hypoxia due to inadequate numbers of oxygen-bearing erythrocytes.
Activity intolerance is a common problem for patients with anemia. Physical activity increases demand for oxygen, but if there are not enough circulating erythrocytes to provide sufficient oxygen, patients become physically weak and unable to engage in normal physical activity without experiencing profound fatigue. This can result in some degree of
self-care deficit as the fatigue interferes with the patient's ability to carry on regular or enjoyable activities.
autoimmune hemolytic anemia (AIHA) an acquired disorder characterized by hemolysis due to the production of autoantibodies against one's own red blood cell antigens.
congenital hypoplastic anemia drug-induced hemolytic anemia (
drug-induced immune hemolytic anemia) a form of
immune hemolytic anemia induced by the taking of drugs, involving one of four different mechanisms:
Immune complex problems: Ingestion of any of a large number of drugs is followed by immunization and the formation of a soluble drug–anti-drug complex that adsorbs nonspecifically to the erythrocyte surface.
Drug absorption: Drugs bind firmly to erythrocyte membrane proteins, inducing the formation of specific antibodies; the drug most commonly associated with this mechanism is penicillin.
Membrane modification: A nonimmunologic mechanism whereby the drug involved is able to modify erythrocytes so that plasma proteins can bind to the membrane.
Autoantibody formation: Methyldopa (Aldomet) induces the production of autoantibodies that recognize erythrocyte antigens and are serologically indistinguishable from those seen in patients with warm autoimmune hemolytic anemia.
hypochromic anemia anemia in which the decrease in hemoglobin is proportionately much greater than the decrease in number of erythrocytes.
hypochromic microcytic anemia any anemia with
microcytes that are hypochromic (reduced in size and in hemoglobin content); the most common type is
iron deficiency anemia. hypoplastic anemia anemia due to incapacity of blood-forming organs.
iron deficiency anemia a type of
hypochromic microcytic anemia that results from the presence of greater demands on stored
iron than can be met, usually because of chronic blood loss, dietary deficiency, or defective absorption; it is characterized by low or absent iron stores, low serum iron concentration, low
transferrin saturation, elevated transferrin (total iron-binding capacity), and low
hemoglobin concentration or
hematocrit. Iron deficiency anemia is the most common nutritional disorder in the United States.
macrocytic anemia anemia characterized by
macrocytes (erythrocytes much larger than normal).
megaloblastic anemia any of various anemias characterized by the presence of
megaloblasts in the bone marrow or blood; the most common type is
pernicious anemia.
normochromic anemia that in which the hemoglobin content of the red blood cells is in the normal range.
normocytic anemia anemia characterized by proportionate decrease in hemoglobin, packed red cell volume, and number of erythrocytes per cubic millimeter of blood.
nutritional anemia anemia due to a deficiency of an essential substance in the diet, which may be caused by poor dietary intake or by malabsorption; called also
deficiency anemia.
sideroachrestic anemia (
sideroblastic anemia) any of a heterogenous group of acquired and hereditary anemias with diverse clinical manifestations, commonly characterized by large numbers of
sideroblasts in the bone marrow, ineffective erythropoiesis, variable proportions of hypochromic erythrocytes in the peripheral blood, and usually increased levels of tissue iron.
spur cell anemia anemia in which the erythrocytes are acanthocytes (spur cells) and are destroyed prematurely, primarily in the spleen; it is an acquired form occurring in severe liver disease in which there is increased serum cholesterol and increased uptake of cholesterol into the erythrocyte membrane, causing the abnormal shape.
aplastic
[a-plas´tik] pertaining to or characterized by aplasia; having no tendency to develop into new tissue.
aplastic anemia any form of anemia caused by
bone marrow failure or aplasia of the marrow. This may be due to chemical factors such as drugs, to physical factors such as radiation, to infection by a virus, or to idiopathic congenital defects of the stem cells of the bone marrow. It is characterized by a reduction or depletion of hemopoietic precursor cells with decreased production of leukocytes, erythrocytes, and platelets, resulting in peripheral blood
pancytopenia. Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
Ehrlich,
Paul, German bacteriologist, immunologist, and Nobel laureate, 1854-1915. Ehrlichia - a genus of small, often pleomorphic, coccoid to ellipsoidal, nonmotile, gram-negative bacteria (order Rickettsiales) that are the etiologic agents of ehrlichiosis and are transmitted by ticks.
Ehrlich anemia - anemia resulting from hypoplastic or aplastic bone marrow. Synonym(s): aplastic anemia
Ehrlich diazo reagent - two solutions, one of sodium nitrite, the other of acidified sulfanilic acid, used in bringing about diazotization. Synonym(s): diazo reagent
Ehrlich inner body - a round oxyphil body found in the red blood cell in case of hemocytolysis due to a specific blood poison. Synonym(s):
Heinz-Ehrlich body Ehrlich phenomenon - the difference between the amount of diphtheria toxin that will exactly neutralize one unit of antitoxin.
Ehrlich postulate - that cells contain surface extensions or side chains (haptophores) that bind to the antigenic determinants of a toxin (toxophores). Synonym(s): Synonym(s):
Ehrlich theory;
side-chain theory Ehrlich test - urobilinogen test using Ehrlich reagent.
Ehrlich tumor - solid or ascitic transplantable tumor derived from breast carcinoma in mice.
Ehrlich unit
Ehrlich-Türk line - seldom-used term for the thin vertical deposition of material on the posterior surface of the cornea seen in uveitis.
Medical Eponyms © Farlex 2012